A nurse is caring for a client who has dementia and is scheduled for a procedure. Which of the following individuals should the nurse request to sign the client's informed consent?
The client's son, who has a durable power of attorney.
The client's sister, who assists with finances.
The client's daughter, who is the primary caregiver.
The client, who has advance directives.
The Correct Answer is A
The nurse should request the client's son, who has a durable power of attorney, to sign the client's informed consent. A durable power of attorney is a legal document that allows an individual to appoint someone to make decisions on their behalf in the event that they become unable to do so. If the client has dementia and is unable to provide informed consent for the procedure, the individual with a durable power of attorney has the legal authority to make decisions on their behalf.
The other individuals are not the appropriate person to sign the client's informed consent. The client's sister [b] and daughter [c] may be involved in the client's care and decision-making, but they do not have the legal authority to provide informed consent on behalf of the client unless they have been designated as such in a legal document. Advance directives [d] are legal documents that allow individuals to communicate their wishes about medical treatment and end-of-life care, but they do not grant decision-making authority to another individual.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
The charge nurse is demonstrating the right of supervision by checking with other nursing personnel on the unit throughout the day to determine if they are completing tasks. This means that the charge nurse is providing appropriate supervision and monitoring of the delegated tasks to ensure that they are being completed correctly and that the client's needs are being met.
Option B is incorrect because it refers to ensuring that the circumstances are appropriate for delegation.
Option C is incorrect because it refers to delegating tasks to the right person who has the appropriate skills and knowledge to complete them.
Option D is incorrect because it refers to clear communication between the delegator and delegatee about the task being delegated.

Correct Answer is ["A","B","C","E"]
Explanation
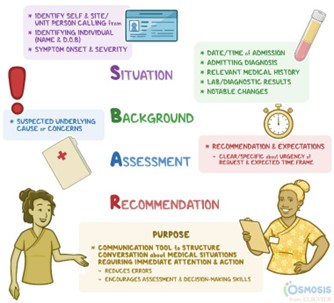
SBAR stands for Situation, Background, Assessment, and Recommendation. It is a systematic method of communication that provides a structured framework for conveying important information about a patient. To ensure that the report is thorough, the nurse needs to include information about the situation of the patient, the background leading up to the situation, an assessment of the patient, and recommendations for moving forward.
Option d is incorrect because barriers to providing treatment are not part of the SBAR framework.
Option f is incorrect because the reason why the report is needed is not part of the SBAR framework.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
