The nurse is completing an assessment on a client suspected of having a transient ischemic attack. Which of the following techniques should the nurse use to assess the client's carotid arteries?
Simultaneously palpating both arteries to compare amplitude.
Listening with the diaphragm of the stethoscope to assess for bruits.
instructing the patient to take slow deep breaths during auscultation.
Palpating the artery at the base of the neck of the neck.
The Correct Answer is B
A. Simultaneously palpating both arteries to compare amplitude: While comparing amplitudes is important, using the diaphragm of the stethoscope to listen for bruits (abnormal whooshing sounds indicating turbulent blood flow) is a more specific and accurate method for assessing the carotid arteries for potential vascular issues.
B. Listening with the diaphragm of the stethoscope to assess for bruits: This technique allows the nurse to detect abnormal sounds (bruits) that could indicate partial blockages or stenosis in the carotid arteries, suggesting a risk of stroke or transient ischemic attack.
C. Instructing the patient to take slow deep breaths during auscultation: Deep breaths are more relevant during lung auscultation. Carotid artery assessment focuses on detecting abnormal sounds and assessing blood flow rather than respiratory patterns.
D. Palpating the artery at the base of the neck: Palpation alone does not provide enough information about potential blockages or abnormalities in the carotid arteries. Listening with a stethoscope allows for a more detailed assessment of blood flow and the presence of bruits. f the nurse hears a bruit during auscultation, they should not palpate the carotid artery. A bruit suggests partial obstruction (carotid stenosis), and compressing the artery further could worsen blood flow.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
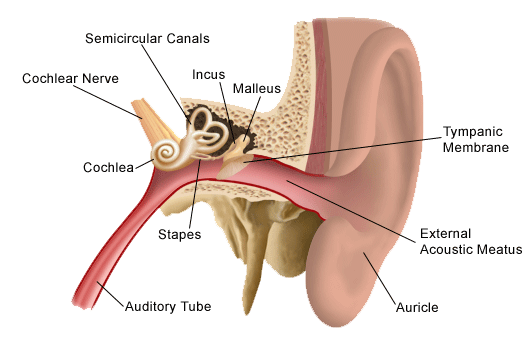
A. Auricle (Pinna):
The auricle, also known as the pinna, is the visible external part of the ear. It consists of movable cartilage and skin. When administering eardrops, pulling the auricle up and back helps to straighten the ear canal, allowing the drops to enter the ear effectively.
B. Mastoid Process:
The mastoid process is a bony prominence located behind the ear. It is not a part of the outer ear structure involved in administering eardrops.
C. Outer Meatus:
The outer meatus, also known as the external acoustic meatus or ear canal, is the tube-like structure leading from the auricle to the eardrum. It is the passage through which eardrops are administered. Pulling the auricle up and back helps to straighten the outer meatus for the proper administration of eardrops.
D. Concha:
The concha refers to the bowl-shaped depression next to the ear canal. While it is a part of the outer ear, pulling the concha is not a technique used for administering eardrops. The auricle, specifically, is manipulated to facilitate the process.
Correct Answer is ["A","B","C","D","E"]
Explanation
A. Use of accessory muscles
Explanation: Using accessory muscles during breathing indicates increased effort to breathe, which can be a sign of respiratory distress. It suggests that the client is having difficulty breathing and is using additional muscles to aid in the process. This finding should be reported to the practitioner for further evaluation.
B. Nail bed greater than 160 degrees
Explanation: A nail bed angle greater than 160 degrees, also known as clubbing, is an abnormal finding and can be associated with chronic respiratory or cardiovascular conditions. It may indicate insufficient oxygenation and should be reported to the practitioner for evaluation.
C. Circumoral cyanosis
Explanation: Circumoral cyanosis, which is a bluish discoloration around the mouth, indicates inadequate oxygenation. It can be a sign of respiratory or cardiac problems and should be reported to the practitioner for further assessment and intervention.
D. Pursed lip breathing
Explanation: Pursed lip breathing is a technique often used by individuals with respiratory difficulties to improve oxygen exchange. However, if it's observed in a person who does not normally use this technique, it could indicate respiratory distress and should be reported to the practitioner for evaluation.
E. Anteroposterior-to-transverse diameter of 1:1
Explanation: An anteroposterior-to-transverse diameter of 1:1 (also known as barrel chest) is an abnormal finding often associated with chronic obstructive pulmonary disease (COPD). It suggests overinflation of the lungs and can impair effective breathing. This finding should be reported to the practitioner for further evaluation.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
