A nurse in an emergency department is caring for a child who reports being sexually abused by a family member. Which of the following actions should the nurse take?
Reassure the child that no one will be told about the abuse.
Ensure that multiple nurses are present for the physical examination.
Explain to the child what will happen when the abuse is reported.
Use leading statements to obtain information from the child.
The Correct Answer is C
This is because the nurse should provide honest and accurate information to the child about the reporting process and the possible outcomes, such as legal actions, investigations, or removal from the home.
This can help the child feel more prepared and less anxious about what will happen next. The nurse should also reassure the child that the abuse is not their fault and that they did the right thing by telling someone.
Choice A is wrong because reassuring the child that no one will be told about the abuse is unethical and illegal.
The nurse has a mandatory duty to report any suspected or confirmed cases of child abuse to the appropriate authorities, such as child protective services or law enforcement. Keeping the abuse a secret can also endanger the child’s safety and well-being, as well as prevent them from receiving the necessary medical and psychological care.
Choice B is wrong because ensuring that multiple nurses are present for the physical examination can increase the child’s fear, embarrassment, or discomfort.
The nurse should minimize the number of people involved in the examination and only include those who are essential for providing care or collecting evidence. The nurse should also explain to the child what will be done during the examination and obtain their consent before proceeding.
Choice D is wrong because using leading statements to obtain information from the child can influence their responses and affect the validity of their testimony.
The nurse should use open-ended questions and avoid suggesting or implying any details about the abuse. The nurse should also document the child’s statements verbatim and avoid interpreting or paraphrasing them.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
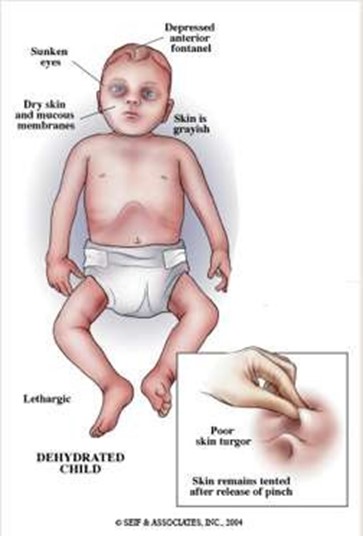
These are signs of severe dehydration in an infant, which can be life-threatening and should be reported to the provider immediately. The infant may need intravenous fluids and electrolytes to restore hydration and prevent complications.
Choice B is wrong because a temperature of 38° C (100.4° F) and a pulse rate of 124/min are not abnormal for an infant and do not indicate severe dehydration. These are common findings in an infant who has gastroenteritis, which is an inflammation of the stomach and intestines caused by a virus, bacteria, or parasite.
Choice C is wrong because decreased appetite and irritability are also common findings in an infant who has gastroenteritis, but they do not indicate severe dehydration. The nurse should encourage oral rehydration with fluids such as breast milk, formula, or oral electrolyte solution.
Choice D is wrong because pale skin and a 24-hr fluid deficit of 30 mL are not signs of severe dehydration in an infant.
A fluid deficit of 30 mL is less than 1 oz and is not significant for an infant who weighs about 10 kg (22 lbs). A fluid deficit of more than 10% of body weight would indicate severe dehydration.
Normal ranges for vital signs in infants are as follows:
• Temperature: 36.5° C to 37.5° C (97.7° F to 99.5° F)
• Pulse rate: 100 to 160/min
• Respiratory rate: 30 to 60/min
• Blood pressure: 65/41 to 100/50 mm Hg
Normal ranges for fluid intake and output in infants are as follows:
• Fluid intake: 100 to 150 mL/kg/day
• Fluid output: 1 to 2 mL/kg/hr
Correct Answer is B
Explanation
The correct answer is Choice B
Choice A rationale: Inserting the catheter without applying suction is correct technique. Suction should only be applied while withdrawing the catheter to prevent mucosal trauma and hypoxia. Initiating suction during insertion can damage tracheal lining and cause bradycardia due to vagal stimulation. Allowing clean insertion without suction reduces injury risk and supports effective secretion removal on withdrawal with controlled suction time.
Choice B rationale: Waiting 2 minutes between suction passes is too long and may delay secretion clearance, risking hypoxia and secretion buildup. Best practice is to wait about 30 seconds to 1 minute or until the client recovers baseline oxygen saturation and heart rate. Prolonged intervals may lead to atelectasis or respiratory distress in patients with poor reserve, especially if suctioning is incomplete or secretions are copious.
Choice C rationale: Suctioning should be limited to 10–15 seconds per pass to reduce hypoxemia and bronchospasm risks. Applying suction for 15 seconds falls within the upper acceptable range, particularly if preoxygenation is done. Extended suction beyond this can decrease PaO₂ levels rapidly. Limiting the suction time ensures safer removal of secretions while minimizing trauma and preserving adequate oxygenation.
Choice D rationale: Encouraging the client to cough facilitates mobilization of secretions toward the upper airway, making suctioning more effective. Coughing also enhances airway clearance naturally and may reduce the number of required suction passes. It is a therapeutic action in tracheostomy care that supports pulmonary hygiene, helps prevent atelectasis, and can reduce the need for deep suctioning interventions.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
