A nurse is caring for a client who has chronic venous insufficiency. Which of the following areas should the nurse assess for the presence of a venous ulcer?
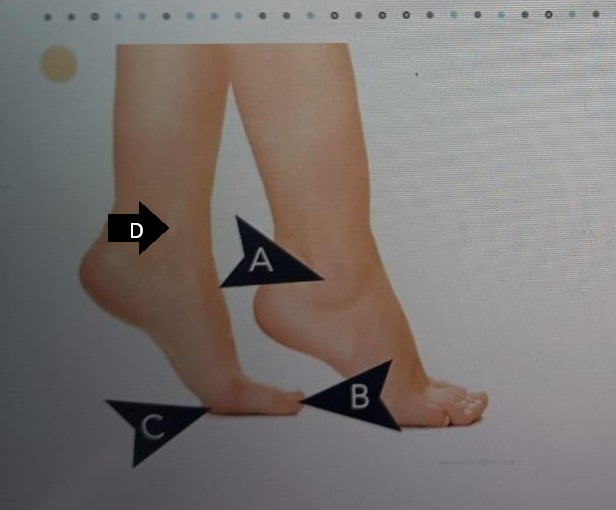
A
B
C
D
The Correct Answer is D
Rationale:
A. This area is the lateral side of the the heel and is more commonly affected by arterial ulcers or pressure injuries. It is not the typical location for ulcers caused by venous insufficiency.
B. This area is the area on the tip of toes and is not a typical site for venous ulcers. Ulcers in this location are commonly arterial or diabetic ulcers.
C. This area is the area on the sole of the feet at the base of the big toe and is not a typical site for venous ulcers.
D. This area is the medial malleolus, just above the inner ankle, which is the most common site for venous ulcers. Chronic venous insufficiency leads to venous stasis and increased pressure in this region, causing skin breakdown and ulceration.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
Rationale:
A. The client's bed has a three-prong plug attached to the electrical cord: A three-prong plug provides grounding and is a standard safety feature. It helps prevent electric shock and is not considered a hazard.
B. A protective cover is inserted into an unused outlet: Outlet covers are recommended, especially in homes with children, to prevent accidental electrical shock. This is a safety measure, not a hazard.
C. An IV pump is plugged into an outlet near a sink: This is a safety hazard because electrical devices should not be used near water sources. The proximity to the sink increases the risk of electrical shock or short-circuiting if moisture contacts the outlet or device.
D. An electrical cord is coiled and secured to the floor: Coiling and securing cords can prevent tripping hazards and is generally acceptable as long as the cord is not damaged or covered in a way that could lead to overheating.
Correct Answer is A
Explanation
Rationale:
A. "I am aware that my diabetes is caused by an autoimmune disorder.": Type 1 diabetes mellitus results from the immune system attacking the insulin-producing beta cells in the pancreas. This autoimmune destruction leads to a complete deficiency of insulin, making lifelong replacement necessary.
B. "I know that my diabetes developed slowly over several years.": Type 1 diabetes often has a rapid onset, especially in younger individuals. Symptoms such as polyuria, polydipsia, weight loss, and fatigue can appear suddenly over days or weeks, rather than gradually over several years.
C. "If I lose weight, I may be able to stop taking insulin.": Weight loss does not eliminate the need for insulin in type 1 diabetes. Because the pancreas no longer produces insulin, insulin therapy remains necessary regardless of changes in body weight or physical condition.
D. "I have developed a resistance to insulin.": Insulin resistance is a feature of type 2 diabetes, where the body produces insulin but cannot use it effectively. In type 1 diabetes, the problem is a lack of insulin production due to the destruction of pancreatic beta cells.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
