A nurse is caring for a client who is in labor. Which of the following nursing actions reflects application of the gate control theory of pain?
Encourage the client to rest between contractions.
Massage the client's back.
Turn the client onto her left side.
Administer prescribed analgesic medication.
The Correct Answer is B
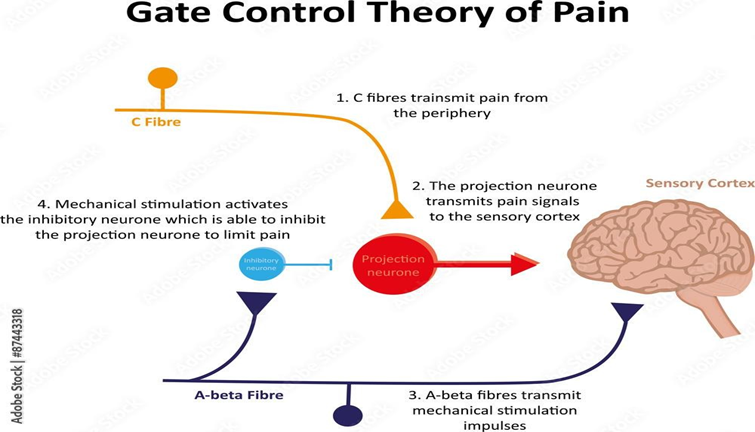
B. Massage can stimulate large-diameter nerve fibers that carry non-painful sensations (such as touch and pressure). Activation of these fibers can help close the gate, reducing the transmission of painful stimuli from smaller pain fibers. Therefore, massaging the client's back aligns with the Gate Control Theory by modulating sensory input to the spinal cord.
A. This action can help distract the client from pain and reduce anxiety, which can potentially close the "gate" and decrease the perception of pain. By promoting relaxation and rest, the nurse may indirectly influence the gating mechanism to inhibit pain signals.
C. Positioning the client can be beneficial during labor for various reasons, such as improving blood flow and easing the labor process. While specific lateral positioning (like the left side) may not directly relate to the Gate Control Theory, it can contribute to overall comfort and relaxation, which can influence pain perception indirectly.
D. While analgesic medication can effectively relieve pain, it operates primarily through chemical modulation of pain receptors and pathways in the nervous system. It does not directly interact with the gate mechanism described by the Gate Control Theory. However, by reducing the intensity of pain signals reaching the brain, it can still alleviate pain experienced by the client.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
D. Hypertension, especially severe and uncontrolled hypertension (chronic or gestational), increases the risk of placental abruption. Elevated blood pressure can lead to vascular changes in the placenta and uterine vessels, predisposing to abruption.
A. Cocaine use is a known risk factor for placental abruption due to its vasoconstrictive effects, which can lead to decreased blood flow to the placenta and increase the risk of abruption. However, it is not common.
B. Cigarette smoking is also a recognized risk factor for placental abruption. Smoking contributes to placental dysfunction and impaired oxygen delivery to the fetus, increasing the risk of abruption.
C. Trauma, such as from motor vehicle accidents or physical assaults, is a significant risk factor for placental abruption. The force of impact can cause shearing forces within the uterus, leading to separation of the placenta from the uterine wall.
Correct Answer is B
Explanation
B. Deep tendon reflexes (DTRs) are commonly decreased in preeclampsia rather than increased. A +1 response suggests normal or slightly increased reflexes, which is not typically seen in preeclampsia. Instead, hyperreflexia (brisk reflexes) or even clonus (repetitive and rhythmic movements) may be present due to central nervous system irritability associated with severe preeclampsia or eclampsia.

A. Preeclampsia can cause generalized edema, including pitting edema in various parts of the body, due to fluid retention. Edema, especially in the sacral area, is consistent with preeclampsia and occurs due to increased capillary permeability and fluid shifts.
C. Hypertension (elevated blood pressure) is a hallmark of preeclampsia. A blood pressure reading of 148/98 mm Hg is consistent with preeclampsia, especially considering the systolic (top number) is elevated above 140 mm Hg.
D. Proteinuria (protein in the urine) is another key diagnostic criteria for preeclampsia. The grading of proteinuria is typically done on a scale from trace (±) to 4+ (marked). 3+ protein in the urine indicates significant proteinuria, which is consistent with preeclampsia and reflects kidney involvement.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
