A nurse is caring for an infant who has gastroenteritis.
Which of the following assessment findings should the nurse report to the provider?
Sunken fontanels and dry mucous membranes.
Temperature 38° C (100.4° F) and pulse rate 124/min.
Decreased appetite and irritability.
Pale and a 24-hr fluid deficit of 30 mL.
The Correct Answer is A
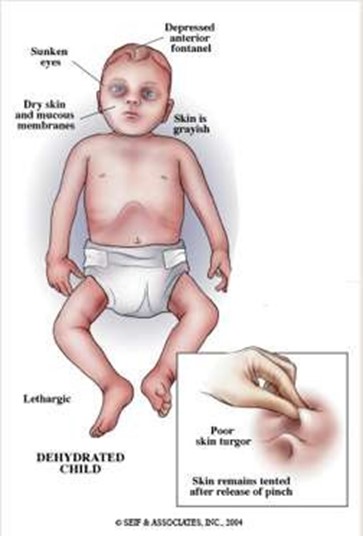
These are signs of severe dehydration in an infant, which can be life-threatening and should be reported to the provider immediately. The infant may need intravenous fluids and electrolytes to restore hydration and prevent complications.
Choice B is wrong because a temperature of 38° C (100.4° F) and a pulse rate of 124/min are not abnormal for an infant and do not indicate severe dehydration. These are common findings in an infant who has gastroenteritis, which is an inflammation of the stomach and intestines caused by a virus, bacteria, or parasite.
Choice C is wrong because decreased appetite and irritability are also common findings in an infant who has gastroenteritis, but they do not indicate severe dehydration. The nurse should encourage oral rehydration with fluids such as breast milk, formula, or oral electrolyte solution.
Choice D is wrong because pale skin and a 24-hr fluid deficit of 30 mL are not signs of severe dehydration in an infant.
A fluid deficit of 30 mL is less than 1 oz and is not significant for an infant who weighs about 10 kg (22 lbs). A fluid deficit of more than 10% of body weight would indicate severe dehydration.
Normal ranges for vital signs in infants are as follows:
• Temperature: 36.5° C to 37.5° C (97.7° F to 99.5° F)
• Pulse rate: 100 to 160/min
• Respiratory rate: 30 to 60/min
• Blood pressure: 65/41 to 100/50 mm Hg
Normal ranges for fluid intake and output in infants are as follows:
• Fluid intake: 100 to 150 mL/kg/day
• Fluid output: 1 to 2 mL/kg/hr
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is {"A":{"answers":"A"},"B":{"answers":"B"},"C":{"answers":"A"},"D":{"answers":"A"},"E":{"answers":"B"}}
Explanation
Answer is… Stay with the client for the first 15 min of the transfusion and Document the blood product transfusion in the client’s medical record are indicated nursing actions for the client. Obtain the first unit of packed RBCs from the blood bank is also indicated, but it should be done before starting the transfusion. Titrate the rate of infusion to maintain the client’s blood pressure at least 90/60 mm Hg and Start an IV bolus of lactated Ringer’s solution are not indicated nursing actions for the client.
Explanation:.
- Staying with the client for the first 15 min of the transfusion is indicated because this is when most adverse reactions occur and the nurse should monitor the client’s vital signs and symptoms closely.
- Documenting the blood product transfusion in the client’s medical record is indicated because this is part of the legal and ethical responsibility of the nurse and it provides a record of the type, amount, duration, and outcome of the transfusion.
- Obtaining the first unit of packed RBCs from the blood bank is indicated because this is part of the preparation for the transfusion and it ensures that the blood product is compatible, fresh, and available. However, this should be done before starting the transfusion, not after.
- Titrating the rate of infusion to maintain the client’s blood pressure at least 90/60 mm Hg is not indicated because this may cause fluid overload or hemolysis in the client who already has a low blood pressure and a high heart rate. The rate of infusion should be based on the client’s condition, weight, and response to the transfusion, not on a fixed target.
- Starting an IV bolus of lactated Ringer’s solution is not indicated because this may cause electrolyte imbalance or hemolysis in the client who already has a positive H. pylori test and a history of gastrointestinal bleeding. The only fluid that should be infused with blood products is 0.9% NaCl (normal saline) because it has a similar osmolarity and pH as blood and it prevents clotting or hemolysis.
Correct Answer is B
Explanation
Determine the client’s knowledge about diaphragm use. This is the first action the nurse should take because it allows the nurse to assess the client’s readiness to learn, identify any knowledge gaps, and tailor the teaching to the client’s needs.
Some of the other choices are wrong because:
Choice A is wrong because Supervise return demonstration of diaphragm use.
This is not the first action the nurse should take because it assumes that the client already knows how to use the diaphragm correctly and safely. The nurse should first teach the client how to insert, remove, and care for the diaphragm before asking for a return demonstration.
Choice C is wrong because Document the client’s level of understanding about potential adverse effects.
This is not the first action the nurse should take because it is part of the evaluation phase of teaching, not the assessment phase. The nurse should first determine what the client knows and needs to know about diaphragm use and its possible risks and benefits.
Choice D is wrong because Teach the client how to insert the diaphragm.
This is not the first action the nurse should take because it is part of the implementation phase of teaching, not the assessment phase. The nurse should first assess the client’s knowledge, motivation, and preferences before providing instruction on how to use the diaphragm.
A contraceptive diaphragm is a birth control device that prevents sperm from entering the uterus.
It is a small, soft silicone or rubber cup with a flexible rim that covers the cervix.
It is inserted into the vagina with spermicide before sex and is held in place by the pelvic muscles. It is a reusable type of contraception that women can use to avoid getting pregnant.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
