A parent calls a clinic and reports to a nurse that his 2-month-old infant is hungry more than usual but is projectile vomiting immediately after eating. Which of the following responses should the nurse make?
"Bring your baby into the clinic today."
"Give your infant an oral rehydration solution."
"Burp your baby more frequently during feedings."
"Try switching to a different formula."
The Correct Answer is A
Choice A: This response is appropriate, as it indicates urgency and concern for the infant's condition. Projectile vomiting immediately after eating can be a sign of pyloric stenosis, which is a condition that causes the narrowing of the pylorus, which is the opening between the stomach and the small intestine. Pyloric stenosis can prevent food from passing through and cause dehydration, electrolyte imbalance, or weight loss. The infant needs to be evaluated by a provider as soon as possible and may need surgery to correct the problem.
Choice B: This response is not appropriate, as it does not address the underlying cause of the infant's condition. Oral rehydration solution can help replace fluids and electrolytes lost through vomiting, but it does not treat pyloric stenosis or prevent further vomiting. Oral rehydration solution may also be vomited out by the infant if given too soon or too much.
Choice C: This response is not appropriate, as it does not address the underlying cause of the infant's condition. Burping the baby more frequently during feedings can help release air bubbles and prevent gas or colic, but it does not treat pyloric stenosis or prevent further vomiting. Burping may also trigger vomiting by increasing pressure on the stomach.
Choice D: This response is not appropriate, as it does not address the underlying cause of the infant's condition. Switching to a different formula can help if the infant has an allergy or intolerance to certain ingredients in their current formula, but it does not treat pyloric stenosis or prevent further vomiting. Switching formulas may also cause diarrhea or constipation by changing the infant's bowel flora.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
Choice A: The Oucher pain scale is not suitable for a 6-month-old infant, as it is designed for children aged 3 to 13 years who can point to pictures of faces that match their pain level. A 6-month-old infant cannot communicate verbally or point to pictures.
Choice B: The FLACC pain scale is suitable for a 6-month-old infant, as it is designed for infants and children aged 2 months to 7 years who cannot verbalize their pain. The FLACC pain scale assesses five behavioral indicators of pain: face, legs, activity, cry, and consolability. Each indicator is scored from 0 to 2 based on the observation of the nurse. The total score ranges from 0 to 10, with higher scores indicating more pain.
Choice C: The FACES pain scale is not suitable for a 6-month-old infant, as it is designed for children aged 3 years and older who can select a face that matches their pain level. A 6-month-old infant cannot communicate verbally or select a face.
Choice D: The Visual Analog Scale (VAS) is not suitable for a 6-month-old infant, as it is designed for adults and older children who can mark a point on a line that represents their pain level. A 6-month-old infant cannot communicate verbally or mark a point on a line.
Correct Answer is A
Explanation
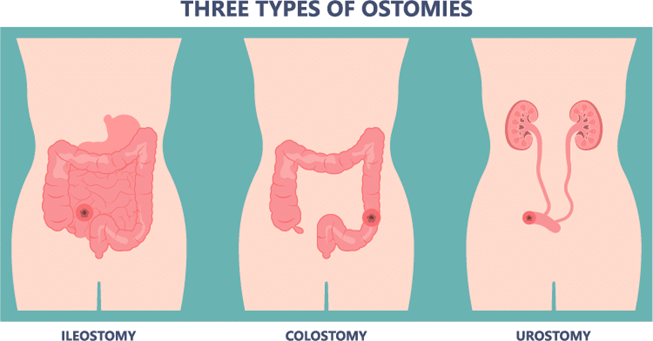
Choice A: An ostomy is a surgical opening in the abdomen that allows stool to pass out of the body. A child who has Hirschsprung disease, which is a condition that causes a blockage of the large intestine due to a lack of nerve cells, may need an ostomy to relieve the obstruction and prevent complications. The ostomy is usually temporary and can be reversed after the affected part of the intestine is removed or repaired. This statement indicates an understanding of the teaching, as the parent knows that the ostomy is not permanent.
Choice B: A urinary catheter is a tube that drains urine from the bladder. A child who has Hirschsprung disease does not need a urinary catheter, as their condition does not affect their urinary system. This statement indicates a lack of understanding of the teaching, as the parent is confused about the type of surgery or device that their child will have.
Choice C: A feeding tube is a tube that delivers nutrition directly into the stomach or small intestine. A child who has Hirschsprung disease may need a feeding tube if they have severe malnutrition, dehydration, or infection due to their condition. However, this is not always necessary and depends on the individual case and the surgeon's preference.
This statement indicates a lack of understanding of the teaching, as the parent assumes that their child will need a feeding tube without knowing the specific plan.
Choice D: A child who has Hirschsprung disease will not have normal bowel movements after the initial surgery, as they will still have an ostomy that bypasses their large intestine. They will need another surgery to reconnect their intestine and restore their bowel function. This statement indicates a lack of understanding of the teaching, as the parent has unrealistic expectations about the outcome of the surgery.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
