A patient diagnosed with electrolyte imbalance induced ventricular tachycardia questions the need for more bananas in their diet.
What is the best information the nurse can give the patient?
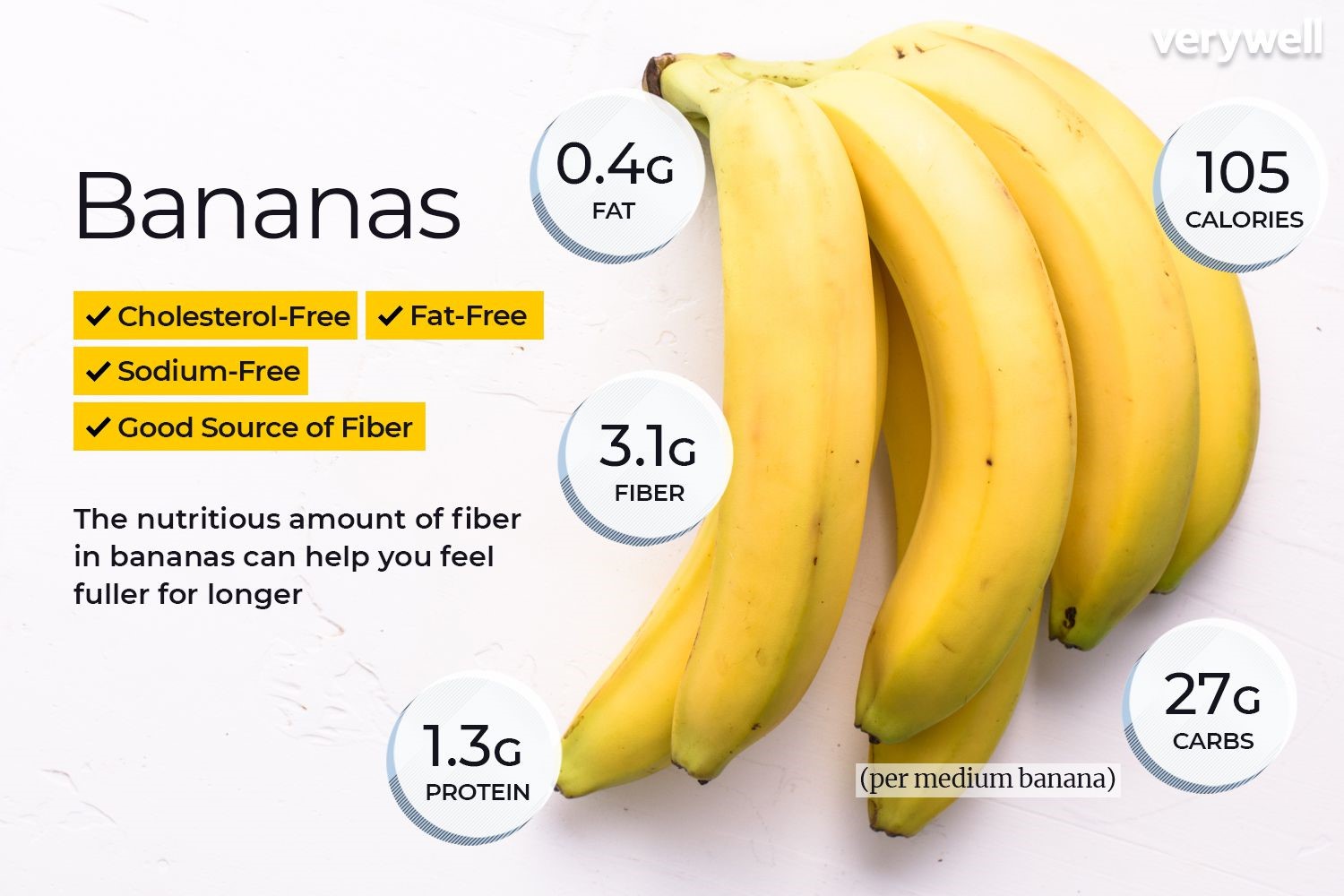
Bananas are high in fiber.
Bananas are high in manganese.
Bananas are low in sodium.
Bananas are high in potassium.
The Correct Answer is D
Choice A rationale:
While bananas do contain fiber, which is beneficial for digestive health and can help regulate blood sugar levels, it is not the most relevant information for a patient with electrolyte imbalance induced ventricular tachycardia. The primary focus should be on addressing the electrolyte imbalance, specifically potassium levels.
Choice B rationale:
Bananas do contain manganese, an essential mineral that plays a role in bone health, metabolism, and wound healing. However, manganese is not directly involved in regulating electrolytes or heart rhythm. Therefore, it's not the most pertinent information for this patient's condition.
Choice C rationale:
While it's true that bananas are relatively low in sodium, this information is not as crucial for a patient with electrolyte imbalance induced ventricular tachycardia. Potassium, not sodium, is the electrolyte that's most likely to be deficient in this condition and needs to be addressed.
Choice D rationale:
Bananas are an excellent source of potassium, a crucial electrolyte that plays a vital role in regulating heart rhythm, muscle contractions, and nerve function. Potassium deficiency, or hypokalemia, can lead to various cardiac arrhythmias, including ventricular tachycardia. Therefore, increasing potassium intake through dietary sources like bananas can be an effective strategy to help manage electrolyte imbalance and potentially reduce the risk of arrhythmias.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
Choice B rationale:
It is crucial to ensure that no one is touching the client during defibrillation to prevent accidental electrical shock to others. The electrical current delivered by the defibrillator is extremely powerful and can cause serious injury or even death if it passes through another person's body. This includes both healthcare professionals and bystanders.
Here are key points to emphasize this rationale:
Electrical conduction: The human body is a good conductor of electricity. If someone is touching the client during defibrillation, the electrical current from the defibrillator can easily pass through their body, potentially causing harm.
Cardiac rhythm disruption: Any contact with the client during shock delivery can interfere with the defibrillator's ability to accurately assess the client's heart rhythm and deliver the appropriate shock. This could potentially worsen the client's condition.
Muscle contractions: The electrical current from the defibrillator can cause involuntary muscle contractions. If someone is touching the client, these contractions could cause them to jerk or move suddenly, potentially causing injury to themselves or others.
Safety guidelines: It is a standard safety guideline in all healthcare settings to clear the area around a client before defibrillation to ensure the safety of everyone involved.
I'll now address the other choices, even though they are not the correct answer, to provide a comprehensive understanding:
Choice A rationale:
While ventilation is important during cardiac arrest, it should be temporarily paused during defibrillation. The chest compressions and electrical shock can cause movement of air in the lungs, which can interfere with the effectiveness of the defibrillation. Additionally, the risk of accidental shock to the person providing ventilation is increased if they are close to the client during defibrillation.
Choice C rationale:
Waiting 3 minutes between shocks is not necessary with modern defibrillators. Current guidelines recommend immediate defibrillation for shockable rhythms such as ventricular fibrillation or pulseless ventricular tachycardia. Delaying defibrillation can decrease the chances of successful resuscitation.
Choice D rationale:
The placement of gel pads is important for effective conduction, but it is not the priority action during defibrillation. Ensuring safety by clearing the area and delivering the shock promptly is more critical in the initial moments of defibrillation.
Correct Answer is ["A","B","D"]
Explanation
Choice A rationale:
Pain relief is a primary benefit of morphine administration in the setting of myocardial infarction.
Pain can trigger a stress response, leading to increased heart rate, blood pressure, and myocardial oxygen demand.
Morphine effectively reduces pain, thereby lessening the stress response and its detrimental effects on the heart.
This helps to minimize myocardial ischemia and potential further damage to the heart muscle.
Pain control also improves patient comfort and overall well-being, which can indirectly contribute to better cardiac outcomes.
Choice B rationale:
Sedation is another important benefit of morphine in this context.
It promotes rest and relaxation, which can lower heart rate, blood pressure, and myocardial oxygen demand.
This is crucial for patients with myocardial infarction, as their hearts require reduced workload to heal and recover.
Sedation also helps to alleviate anxiety and agitation, which can further strain the heart.
By inducing a state of calmness, morphine can indirectly protect the heart from additional stress.
Choice C rationale:
While morphine does have diuretic effects, increasing urinary output is not a primary goal in the management of myocardial infarction.
In fact, excessive diuresis could potentially lead to dehydration and hypotension, which could be detrimental to cardiac function.
Therefore, while morphine may slightly increase urine output, this is not a major reason for its use in this setting.
Choice D rationale:
Decreasing myocardial demand is a key benefit of morphine administration in patients with myocardial infarction.
Morphine achieves this by:
Reducing pain and the associated stress response
Promoting sedation and relaxation
Diminishing anxiety and agitation
Exerting a direct vasodilatory effect on blood vessels
This collective action of morphine leads to a decrease in heart rate, blood pressure, and the heart’s overall workload.
As a result, the heart requires less oxygen and experiences reduced strain, allowing for better healing and recovery following a myocardial infarction.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
