A patient is admitted to the hospital with SOB. The nurse notices increasing confusion and combativeness during the past hour. Which of the following actions is appropriate first?
Assess the patient; check to see if the oxygen is flowing correctly
Page the MD STAT
Put up the patient's side rails and apply soft restraints
Administer an IM sedative
The Correct Answer is A
A. Assess the patient; check to see if the oxygen is flowing correctly:
This option involves assessing the patient's condition promptly, particularly focusing on the adequacy of oxygenation. Checking the oxygen delivery system ensures that the patient is receiving the prescribed oxygen therapy at the appropriate flow rate. In a patient with shortness of breath (SOB) and increasing confusion and combativeness, hypoxemia (low oxygen levels) could be a contributing factor. Therefore, assessing the oxygen delivery system is crucial to ensure proper oxygenation and address potential causes of the patient's symptoms.
B. Page the MD STAT:
Paging the MD STAT may be necessary after assessing the patient's condition, especially if the patient's symptoms indicate a medical emergency or require immediate intervention. However, in this scenario, the priority is to assess the patient's condition and address any immediate concerns related to oxygenation and respiratory status. While paging the healthcare provider may be necessary, it should not delay the initial assessment and interventions needed to stabilize the patient.
C. Put up the patient's side rails and apply soft restraints:
Applying side rails and soft restraints should not be the first action in response to the patient's symptoms. While patient safety is important, these measures should only be implemented after other interventions have been attempted, and there is a risk of harm to the patient or others due to agitation or combativeness. In this case, the patient's confusion and combativeness may be secondary to hypoxemia, so addressing oxygenation and assessing the patient's condition are the immediate priorities.
D. Administer an IM sedative:
Administering a sedative should not be the first action in this scenario. Sedation may be considered if the patient's agitation or combativeness poses a risk to their safety or interferes with assessment and treatment. However, the underlying cause of the patient's symptoms, such as hypoxemia, should be addressed first. Administering a sedative without addressing the potential cause of the patient's symptoms could mask important clinical indicators and delay appropriate treatment.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
A. Treatment is not needed if the client is asymptomatic.
Even asymptomatic pulmonary embolisms can lead to complications such as progression to symptomatic PE or development of chronic thromboembolic pulmonary hypertension. Therefore, treatment is necessary to prevent these complications.
B. Treatment is not needed if the pulmonary embolism is intermediate.
The severity of a pulmonary embolism is determined by various factors, including the size and location of the clot and the degree of obstruction in the pulmonary arteries. Intermediate-risk pulmonary embolisms still require treatment to prevent complications and reduce the risk of progression to a more severe or life-threatening condition.
C. Treatment is not needed if the client is hemodynamically stable.
Hemodynamic stability refers to the client's circulatory status and whether they are maintaining adequate blood flow to vital organs. While hemodynamically stable clients may not require aggressive interventions such as thrombolytic therapy or surgical embolectomy, they still require anticoagulant therapy to prevent further clot formation and reduce the risk of complications.
D. Treatment is needed for all clients who have a pulmonary embolism.
Pulmonary embolism (PE) is a serious and potentially life-threatening condition that requires prompt treatment. Regardless of the severity of symptoms or the client's hemodynamic stability, treatment is necessary to prevent complications and reduce the risk of recurrence. Treatment typically includes anticoagulant therapy to prevent further clot formation and may include additional interventions such as thrombolytic therapy or surgical interventions in certain cases.
Correct Answer is C
Explanation
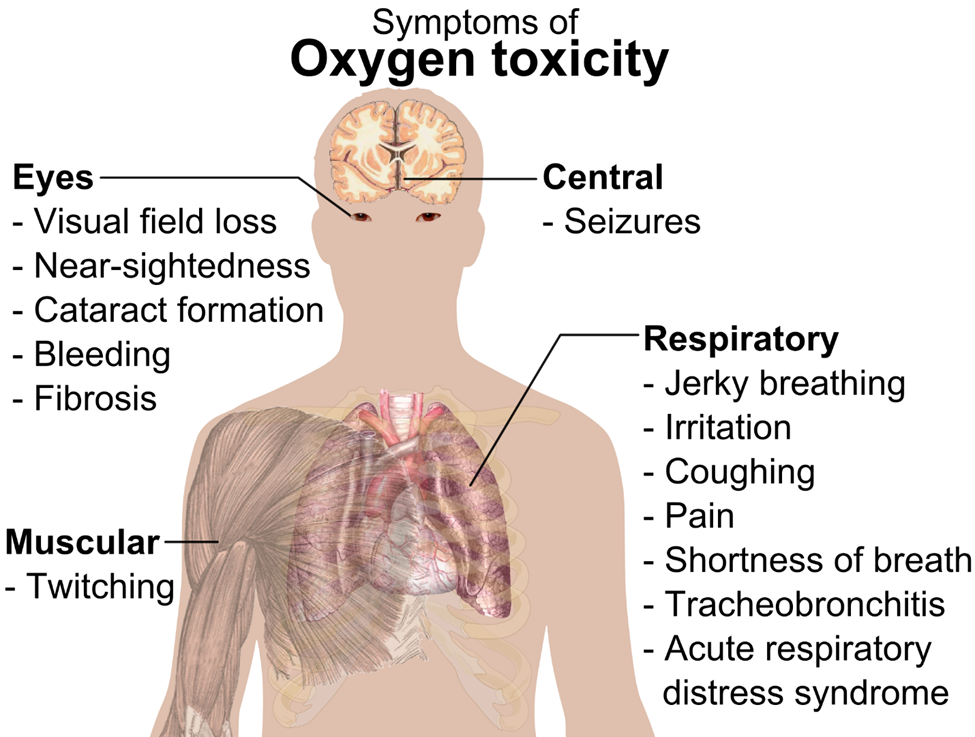
A. Muscle twitching
Muscle twitching is not a typical manifestation of oxygen toxicity. Instead, muscle twitching may be indicative of other conditions such as electrolyte imbalances (e.g., hypocalcemia or hypomagnesemia), neuromuscular disorders, or overstimulation of the nervous system.
B. Metallic taste in mouth
A metallic taste in the mouth is not commonly associated with oxygen toxicity. Instead, a metallic taste in the mouth may occur as a side effect of certain medications, dental issues, or as a symptom of other medical conditions such as acid reflux or oral infections.
C. Facial flushing
Facial flushing is a characteristic finding in oxygen toxicity. When exposed to high levels of oxygen over an extended period, individuals may experience facial flushing due to the vasodilatory effects of oxygen on blood vessels. This dilation of blood vessels leads to increased blood flow to the face, resulting in flushing or reddening of the skin.
D. Periorbital edema
Periorbital edema, or swelling around the eyes, is not a typical manifestation of oxygen toxicity. Instead, periorbital edema may occur as a result of various other conditions such as allergies, sinusitis, or fluid retention. It is not directly related to exposure to high levels of oxygen.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
