Patient Data
Drag from the choices area to specify which condition the client is most likely experiencing, two actions the nurse should take to address that condition, and two parameters the nurse should monitor to assess the client’s progress.
The Correct Answer is []
For Potential Conditions:
The correct answer is c) Abdominal compartment syndrome.
Choice A reason: Pneumothorax is a condition where air leaks into the pleural space, causing lung collapse and impaired gas exchange. It can cause respiratory distress, hypoxia, chest pain, and decreased breath sounds on the affected side. However, it does not cause abdominal distension, acidosis, or hyperglycemia.
Choice B reason: Pulmonary embolism is a condition where a blood clot blocks one or more pulmonary arteries, causing impaired gas exchange and reduced blood flow to the lungs. It can cause respiratory distress, hypoxia, chest pain, and tachycardia. However, it does not cause abdominal distension, acidosis, or hyperglycemia.
Choice C reason: Abdominal compartment syndrome is a condition where increased intra-abdominal pressure causes reduced blood flow to the abdominal organs and impaired diaphragm movement. It can cause respiratory distress, hypoxia, abdominal distension, acidosis, decreased urine output, and organ failure. It is a common complication of cirrhosis with ascites.
Choice D reason: Sepsis is a condition where a systemic inflammatory response to an infection causes organ dysfunction and hypoperfusion. It can cause respiratory distress, hypoxia, fever or hypothermia, tachycardia, acidosis, and hyperglycemia. However, it does not cause abdominal distension unless there is an intra-abdominal infection.
The two actions the nurse should take to address abdominal compartment syndrome are:
- Prepare the client for a paracentesis: Paracentesis is a procedure where a needle or catheter is inserted into the peritoneal cavity to drain excess fluid and reduce intra-abdominal pressure.
- Place an intravenous line to start fluid boluses: Fluid boluses are given to maintain adequate blood pressure and perfusion to the vital organs.
The two parameters the nurse should monitor to assess the client’s progress are:
- Oxygen saturation: Oxygen saturation reflects the amount of oxygen bound to hemoglobin in the blood. It should be maintained above 90% to ensure adequate oxygen delivery to the tissues.
- Urine output: Urine output reflects the function of the kidneys and the perfusion of the renal arteries. It should be maintained above 0.5 mL/kg/hour to prevent acute kidney injury and electrolyte imbalances.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
Choice A reason: This is incorrect because reviewing the need for pneumococcal vaccine is not the most important intervention for the nurse to implement. Pneumococcal vaccine is recommended for people who are at high risk of pneumococcal infections, such as those with chronic diseases or immunosuppression. However, it is not a priority action for a client with neutropenia, which is a low number of neutrophils that increases the risk of bacterial and fungal infections.
Choice B reason: This is incorrect because implementing bleeding precautions is not the most important intervention for the nurse to implement. Bleeding precautions are indicated for clients who have thrombocytopenia, which is a low number of platelets that impairs blood clotting. However, this is not the case for a client with neutropenia, which affects the white blood cells that fight infections.
Choice C reason: This is incorrect because assessing vital signs every 4 hours is not the most important intervention for the nurse to implement. Vital signs are important indicators of the client's health status and may reveal signs of infection, such as fever, tachycardia, or hypotension. However, this is not a sufficient measure to prevent or treat infections in a client with neutropenia, who needs more aggressive and proactive interventions.
Choice D reason: This is correct because placing the client in protective isolation is the most important intervention for the nurse to implement. Protective isolation, also known as reverse isolation or neutropenic precautions, is a set of measures that aim to protect the client from exposure to pathogens that may cause infections. These include wearing gloves, masks, gowns, and eye protection; using sterile equipment and techniques; avoiding contact with people who are sick or have infections; and restricting visitors and fresh flowers or fruits.
Correct Answer is D
Explanation
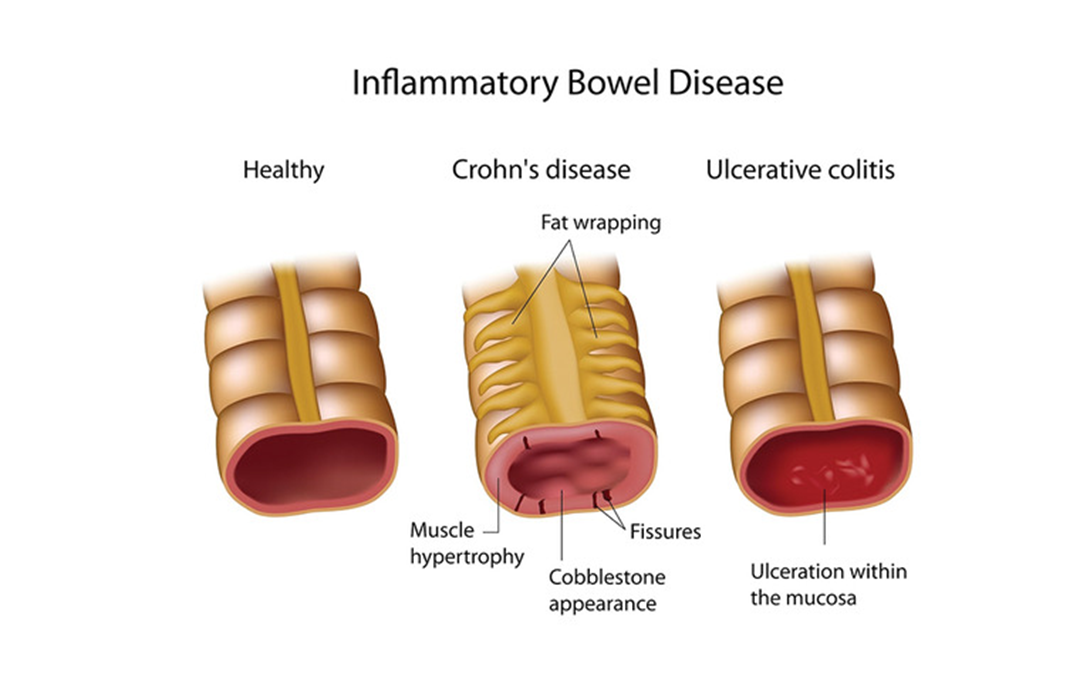
Choice A reason: Measuring capillary glucose level is not a priority action for a client with a rigid abdomen and rebound tenderness. These signs indicate peritonitis, which is a serious complication of IBD that requires immediate attention. Corticosteroids can increase blood glucose levels, but this is not an urgent concern in this situation.
Choice B reason: Encouraging ambulation in the room is not appropriate for a client with a rigid abdomen and rebound tenderness. These signs indicate peritonitis, which is a serious complication of IBD that requires immediate attention. Ambulation can worsen the pain and inflammation, and increase the risk of bowel perforation.
Choice C reason: Monitoring for bloody diarrheal stools is important for a client with IBD, but not a priority action for a client with a rigid abdomen and rebound tenderness. These signs indicate peritonitis, which is a serious complication of IBD that requires immediate attention. Bloody stools can be a sign of ulceration or bleeding in the bowel, but they are not specific to peritonitis.
Choice D reason: Obtaining vital sign measurements is the priority action for a client with a rigid abdomen and rebound tenderness. These signs indicate peritonitis, which is a serious complication of IBD that requires immediate attention. Vital signs can reveal signs of infection, inflammation, shock, and organ failure, which can guide the appropriate interventions and treatments.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
