Following a normal spontaneous vaginal delivery (NSVD), a 28 year old G3 now P3 mother develops sudden onset shortness of breath, hypoxia and cyanosis. The delivery room nurse quickly recognizes these symptoms as possible:
Select one:
Manifestations of uteroplacental insufficiency.
Manifestations of prolapsed cord.
Manifestations of anaphylactoid syndrome of pregnancy.
Manifestations of an acute asthmatic episode.
The Correct Answer is C
Choice A Reason: Manifestations of uteroplacental insufficiency. This is an incorrect answer that describes a different condition that affects the fetus, not the mother. Uteroplacental insufficiency is a condition where the placenta fails to deliver adequate oxygen and nutrients to the fetus, which can result in fetal growth restriction, distress, or demise. Uteroplacental insufficiency does not cause shortness of breath, hypoxia, or cyanosis in the mother.
Choice B Reason: Manifestations of prolapsed cord. This is an incorrect answer that refers to another condition that affects the fetus, not the mother. Prolapsed cord is a condition where the umbilical cord slips through the cervix before the baby and becomes compressed by the fetal head, which can reduce oxygen flow to the fetus. Prolapsed cord does not cause shortness of breath, hypoxia, or cyanosis in the mother.
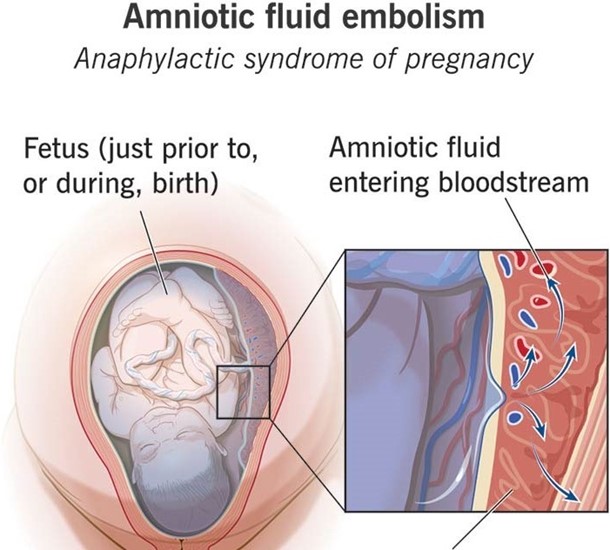
Choice C Reason: Manifestations of anaphylactoid syndrome of pregnancy. This is because anaphylactoid syndrome of pregnancy, also known as amniotic fluid embolism, is a rare and fatal condition where amniotic fluid enters into the maternal bloodstream and causes an allergic reaction, which can lead to respiratory failure, cardiac arrest, coagulopathy, and coma. Anaphylactoid syndrome of pregnancy can occur during or after labor and delivery, especially in cases of NSVD, multiparity, advanced maternal age, or placental abruption.
Choice D Reason: Manifestations of an acute asthmatic episode. This is an incorrect answer that assumes that the mother has a history of asthma or an allergic trigger. Asthma is a chronic inflammatory disorder of the airways that causes wheezing, coughing, chest tightness, and dyspnea. Asthma can be exacerbated by pregnancy or labor, but it is not a common cause of sudden onset respiratory distress in the postpartum period.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
Choice A Reason: Provide compassionate and accurate information throughout the process and support them to make their own decisions. This is a therapeutic strategy that demonstrates empathy, honesty, and advocacy for the couple. It also helps them understand their options, risks, benefits, and alternatives, and encourages them to participate in their care.
Choice B Reason: Inquire about the names they have chosen for their baby to get their mind off their stress. This is a non-therapeutic strategy that avoids addressing the couple's concerns, minimizes their feelings, and may create false hope or unrealistic expectations.
Choice C Reason: Express sympathy and provide directive advice to the couple about what they should do. This is a non-therapeutic strategy that shows pity, imposes personal values, and undermines the couple's self-determination.
Choice D Reason: Refer them to a marriage counselor in the same building to help them with the decisions. This is a non-therapeutic strategy that implies that the couple has marital problems, shifts responsibility, and may create resentment or resistance.
Correct Answer is D
Explanation
Choice A Reason: About 1 of every 5 women will experience abuse in her lifetime is a statistic that shows the prevalence of domestic violence, but it does not address the question of what the nurse should emphasize to the group of women.
Choice B Reason: When women go back to the situation after the abuser has calmed down, things will be beter is a false statement that reflects the cycle of abuse, where the abuser may apologize and promise to change after a violent episode, but then repeat the same behavior later. This does not help the women understand their situation or seek help.
Choice C Reason: The victimized woman can easily leave the situation is a false statement that ignores the many barriers and challenges that women face when trying to escape from domestic violence, such as fear, isolation, financial dependence, lack of support, legal issues, and threats from the abuser. This does not empower the women or provide them with realistic options.
Choice D Reason: The violence will not stop or decrease if the woman becomes pregnant is a true statement that highlights the danger of staying in an abusive relationship during pregnancy. Domestic violence can increase the risk of miscarriage, preterm birth, low birth weight, placental abruption, fetal injury, and maternal death. This may motivate the women to seek safety and protection for themselves and their unborn children.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
