A nurse is caring for a patient on the third day following abdominal surgery.
The nurse notes the absence of bowel sounds, abdominal distention, and the patient has not passed any flatus. Which postoperative complication is the patient likely experiencing?
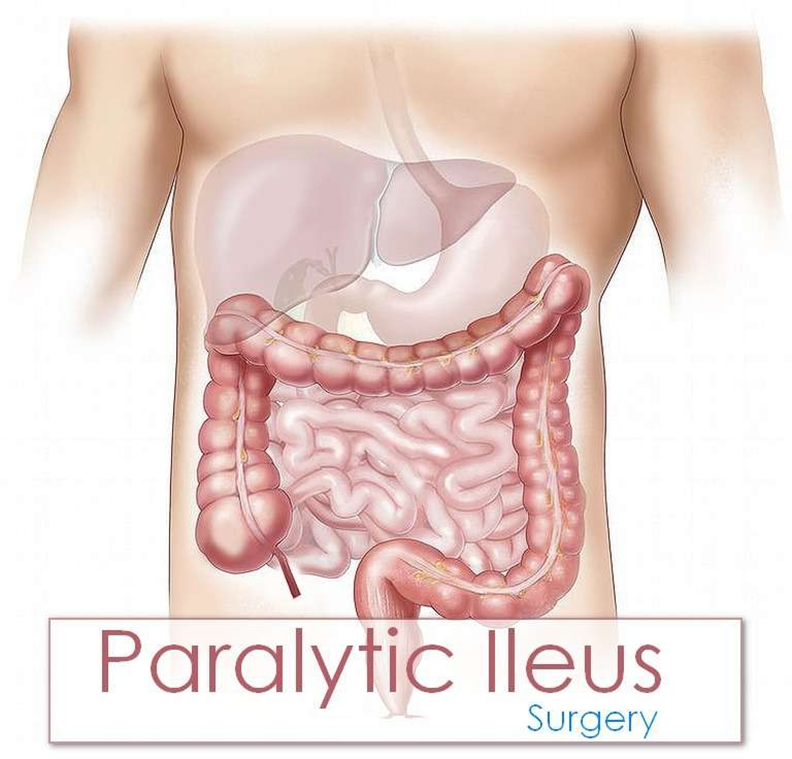
Paralytic ileus
Incisional infection
Fecal impaction
Health care-associated Clostridium difficile
The Correct Answer is A
Choice A rationale:
Paralytic ileus is a common postoperative complication that occurs when the normal movement of the intestines (peristalsis) is slowed or stopped. This can lead to a buildup of gas and fluids in the intestines, causing abdominal distention, nausea, vomiting, and constipation. The absence of bowel sounds, abdominal distention, and the inability to pass flatus are all classic signs of paralytic ileus.
Here are some of the factors that can contribute to paralytic ileus: Manipulation of the intestines during surgery
Anesthesia
Pain medications, especially opioids Electrolyte imbalances
Dehydration
Underlying medical conditions, such as diabetes or kidney disease Treatment for paralytic ileus typically involves:
Resting the bowel by not eating or drinking anything by mouth
Using a nasogastric (NG) tube to suction out gas and fluids from the stomach Providing intravenous (IV) fluids and electrolytes
Encouraging early ambulation
Using medications to stimulate bowel movement, such as metoclopramide or erythromycin
Choice B rationale:
Incisional infection is an infection of the surgical wound. It would typically present with redness, warmth, swelling, and pain at the incision site. The patient may also have a fever. While incisional infections can occur after abdominal surgery, they are not typically associated with the absence of bowel sounds, abdominal distention, and the inability to pass flatus.
Choice C rationale:
Fecal impaction is a severe form of constipation in which a large, hard mass of stool becomes trapped in the rectum. It can cause abdominal pain, bloating, and difficulty passing stool. However, it is not typically associated with the absence of bowel sounds or abdominal distention.
Choice D rationale:
Health care-associated Clostridium difficile (C. difficile) is a bacterial infection that can cause severe diarrhea, abdominal pain, and cramping. It is often associated with antibiotic use. While C. difficile can occur after abdominal surgery, it is not typically associated with the absence of bowel sounds, abdominal distention, and the inability to pass flatus.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
Choice A rationale:
Respiratory acidosis is characterized by a low pH (less than 7.35), a high PaCO2 (greater than 45 mm Hg), and a normal or high HCO3 (22-26 mEq/L). It occurs when there is a buildup of carbon dioxide in the blood due to impaired ventilation.
The patient's ABGs do not align with respiratory acidosis because the pH is elevated (7.6), and the PaCO2 is within the normal range (40 mm Hg).
Choice B rationale:
Respiratory alkalosis is characterized by a high pH (greater than 7.45), a low PaCO2 (less than 35 mm Hg), and a normal or low HCO3 (22-26 mEq/L). It occurs when there is excessive loss of carbon dioxide through hyperventilation.
The patient's ABGs do not align with respiratory alkalosis because the HCO3 is elevated (32 mEq/L), which is not typical for this condition.
Choice C rationale:
Metabolic acidosis is characterized by a low pH (less than 7.35), a normal or low PaCO2 (less than 40 mm Hg), and a low HCO3 (less than 22 mEq/L). It occurs when there is an excess of acid in the body or a loss of bicarbonate.
The patient's ABGs do not align with metabolic acidosis because the pH is elevated (7.6), and the HCO3 is elevated (32 mEq/L).
Choice D rationale:
Metabolic alkalosis is characterized by a high pH (greater than 7.45), a normal or high PaCO2 (40-45 mm Hg), and an elevated HCO3 (greater than 26 mEq/L). It occurs when there is an excess of bicarbonate in the body or a loss of acid.
The patient's ABGs align with metabolic alkalosis because of the high pH (7.6), normal PaCO2 (40 mm Hg), and elevated HCO3 (32 mEq/L).
Correct Answer is ["50"]
Explanation
Here are the steps to calculate the gtt/min for the manual IV infusion:
Step 1: Convert the infusion time from hours to minutes. 8 hours x 60 minutes/hour = 480 minutes
Step 2: Divide the total volume of fluid (in mL) by the infusion time in minutes to get the mL/min rate. 400 mL ÷ 480 minutes = 0.8333 mL/min
Step 3: Multiply the mL/min rate by the drop factor (gtt/mL) to get the gtt/min rate. 0.8333 mL/min x 60 gtt/mL = 50 gtt/min
Therefore, the nurse should set the manual IV infusion to deliver 50 gtt/min.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
