The nurse is teaching the community about blood pressure. What blood pressure finding by the nurse indicates that no changes in therapy are needed for a client with newly diagnosed hypertension?
128/76 mm Hg
128/92 mm Hg
98/56 mm Hg
142/78 mm Hg
The Correct Answer is A
Hypertension is typically diagnosed when a person's blood pressure consistently exceeds 130/80 mm Hg on multiple occasions. However, the specific target blood pressure for treatment may vary based on individual factors and the presence of other comorbidities.
Among the options provided, a blood pressure reading of 128/76 mm Hg is within the target range for many individuals with hypertension. The systolic pressure (128 mm Hg) is below the threshold of 130 mm Hg, and the diastolic pressure (76 mm Hg) is below the threshold of 80 mm Hg.
The other blood pressure readings would warrant further evaluation or possible changes in therapy:
128/92 mm Hg: The diastolic pressure (92 mm Hg) is above the threshold of 80 mm Hg, indicating uncontrolled hypertension.
98/56 mm Hg: This blood pressure reading is below the threshold for hypertension, but it is considered low and may require further assessment to determine if it is normal for the individual or if it indicates hypotension.
142/78 mm Hg: While the systolic pressure (142 mm Hg) is slightly above the threshold of 130 mm Hg, it may not necessarily require immediate changes in therapy. However, it should be closely monitored to ensure blood pressure control.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
Among the given findings, the most important finding to report to the health care provider in a client with a hypertensive emergency is the new-onset blurry vision and facial asymmetry. These symptoms may indicate that the client is experiencing a hypertensive crisis with potential complications such as hypertensive encephalopathy or stroke.
Blurred vision and facial asymmetry are concerning neurological symptoms that suggest possible damage to the blood vessels or organs in the brain. It is crucial to notify the health care provider immediately so that appropriate interventions can be initiated to address the underlying cause and prevent further complications.
While the other findings may also be associated with elevated blood pressure, the new-onset blurry vision and facial asymmetry indicate possible neurological involvement and require immediate attention. Headache, epistaxis (nosebleed), and decreased urine output may be significant symptoms, but the potential neurological implications make the new-onset blurry vision and facial asymmetry the priority for reporting.
Correct Answer is A
Explanation
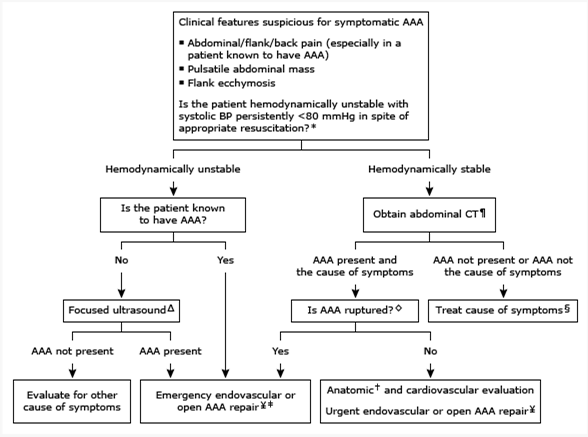
Based on the information provided, the nurse should anticipate that the medical treatment prescribed for a client with an abdominal aortic aneurysm less than 3 cm in size would be regular ultrasound screenings every six (6) months.
Monitoring the size of the abdominal aortic aneurysm through ultrasound is a common approach for managing small aneurysms. Regular ultrasound screenings allow healthcare providers to track the growth rate of the aneurysm and determine if any intervention, such as surgical repair, is necessary as the aneurysm progresses in size.
Let's review the other options and explain why they are not the most appropriate treatments for an abdominal aortic aneurysm less than 3 cm in size:
Intravenous pyelogram yearly: An intravenous pyelogram is an imaging test used to evaluate the urinary system, specifically the kidneys, ureters, and bladder. It is not directly related to the management or monitoring of an abdominal aortic aneurysm.
Assessment of abdominal girth monthly: Assessing the abdominal girth may be a part of the overall assessment of the client's condition, but it is not the primary treatment for managing an abdominal aortic aneurysm. Monitoring the aneurysm size through regular ultrasound screenings is a more specific and accurate approach.
Repair of abdominal aortic aneurysm: Repair of an abdominal aortic aneurysm is typically indicated when the aneurysm reaches a certain size threshold or if it poses a high risk of rupture. For an aneurysm less than 3 cm in size, repair is usually not the initial treatment option. Instead, regular monitoring through ultrasound screenings is recommended to assess the aneurysm's growth rate and determine the appropriate time for intervention.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
