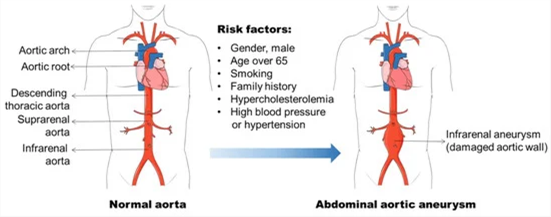
The nurse is caring for a client immediately after repair of an abdominal aortic aneurysm. On assessment, the client has absent popliteal, posterior tibial, and dorsalis pedis pulses. The leg cool and mottled. Which action should the nurse take first?
Wrap both legs in a warming blanket
Compare findings to the preoperative assessment of the pulses
Document the findings and recheck in 15 minutes.
Notify the surgeon and anesthesiologist
The Correct Answer is D
The nurse should prioritize notifying the surgeon and anesthesiologist as the first action. The absent pulses, coolness, and mottled appearance of the leg indicate potential compromised blood flow to the lower extremity, which could be a sign of vascular compromise or acute limb ischemia. These findings are concerning after the repair of an abdominal aortic aneurysm and require immediate medical attention.
Wrap both legs in a warming blanket: While it is important to maintain the client's body temperature, this action alone may not address the underlying issue of compromised blood flow and potential limb ischemia. Notifying the surgeon and anesthesiologist is the priority to address the immediate concern.
Compare findings to the preoperative assessment of the pulses: While comparing findings to the preoperative assessment is important for evaluating the client's condition, it should not delay immediate action. The priority in this situation is to promptly notify the surgeon and anesthesiologist to address the potential vascular compromise.
Document the findings and recheck in 15 minutes: Documenting the findings is an important step in the nursing process, but it should not take precedence over immediate intervention. The concerning signs of absent pulses, coolness, and mottled appearance require urgent attention, and delaying notification could lead to further complications.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
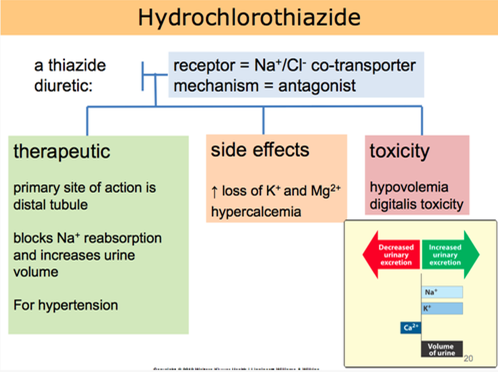
Hydrochlorothiazide is a diuretic medication commonly prescribed for hypertension. It works by increasing urine output, which helps to reduce fluid volume and lower blood pressure. Taking the medication in the morning is beneficial because the increased urine production during the day can help prevent nighttime disruptions due to frequent urination.
Let's go through the other statements and explain why they are not accurate:
"I will not take this medicine when my blood pressure is okay":
This statement indicates a misunderstanding about the purpose of hydrochlorothiazide. It is important to take prescribed medications consistently, even when blood pressure readings are within the normal range, as they are intended to help maintain blood pressure control.
"I will check blood pressure in both arms and legs before taking the drug":
Checking blood pressure in both arms and legs is not directly related to hydrochlorothiazide use. Blood pressure should be monitored regularly, but it is not necessary to perform these measurements specifically before taking the medication.
"I will decrease potassium foods such as bananas in my diet":
Hydrochlorothiazide can cause potassium loss as a side effect. However, reducing potassium-rich foods without healthcare provider guidance may not be appropriate. It is important for the client to discuss dietary adjustments and potassium supplementation with their healthcare provider if needed.
Correct Answer is ["A","C","D","E"]
Explanation
The questions related to the client's history that are most important to ask are:
How would you describe your symptoms?: This question is important to assess the client's current cardiac symptoms and determine the severity, duration, and nature of their symptoms. It helps the nurse to evaluate the client's cardiac status and determine appropriate interventions.
Are you allergic to any medications or foods?: This question is crucial to identify any potential allergies that could impact the client's cardiac care. It helps the nurse ensure that medications and interventions are safe for the client and prevent any adverse reactions.
How did your mother die?:This question is important to gather information about the client's family history of cardiac diseases and potential risk factors. Understanding the family history helps the nurse assess the client's genetic predisposition to cardiac conditions and plan appropriate interventions and screenings.
Have you had shortness of breath or weight gain? : This question is important to assess for symptoms of heart failure or fluid retention. Shortness of breath and weight gain can indicate fluid accumulation, which is a common symptom in cardiac conditions. It helps the nurse evaluate the client's cardiac function and determine the need for furtherinterventions or medication adjustments.
Let's review the other options and explain why they are not the most important questions to ask:
Do you have any children?: While family history is important, specifically asking about children is not as relevant to the client's current cardiac condition. The focus should be on the client's own symptoms, medical history, and family history of cardiac diseases.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
