The school nurse identified 12 students with confirmed cases of influenza A. The families of the children are advised to keep the children home for a minimum of 5 to 7 days. Which of the following is an appropriate action by the nurse?
Discipline in the school setting for improper handwashing.
Education regarding respiratory and hand hygiene.
Running a mandatory flu clinic.
Closing the school for 6 weeks.
The Correct Answer is B
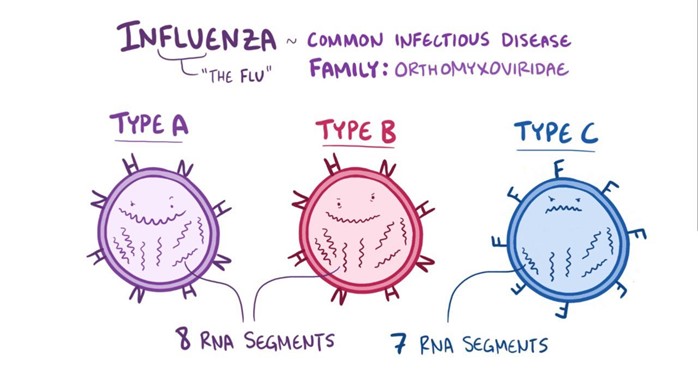
Choice A reason: Discipline in the school setting for improper handwashing is not an appropriate action by the nurse, as it may not prevent the spread of influenza or promote healthy behaviors. Influenza is a viral infection that affects the respiratory system and can be transmitted by direct or indirect contact with respiratory droplets from an infected person. Handwashing is one of the most effective ways to prevent the transmission of influenza and other infectious diseases, but it requires proper technique, frequency, and duration. The nurse should not punish or blame the students for their handwashing habits but rather educate and encourage them to wash their hands with soap and water for at least 20 seconds, especially before and after eating, after using the bathroom, after coughing or sneezing, and after touching potentially contaminated surfaces.
Choice B reason: Education regarding respiratory and hand hygiene is an appropriate action by the nurse, as it helps to prevent the spread of influenza and promote healthy behaviors. The nurse should provide accurate and relevant information to the students, staff, and parents about the causes, symptoms, prevention, and treatment of influenza. The nurse should also teach and demonstrate proper respiratory and hand hygiene practices, such as covering the mouth and nose with a tissue or elbow when coughing or sneezing, disposing of used tissues in a trash can, washing hands frequently with soap and water or using alcohol-based hand sanitizer, avoiding touching the eyes, nose, and mouth, and staying away from sick people.
Choice C reason: Running a mandatory flu clinic is not an appropriate action by the nurse, as it may not be feasible, ethical, or effective in preventing influenza. Influenza vaccination is one of the best ways to prevent influenza and its complications, but it requires informed consent, adequate supply, trained personnel, and appropriate timing. The nurse cannot force or coerce anyone to receive the flu vaccine without their permission or against their wishes. The nurse should respect the autonomy and preferences of the students, staff, and parents, and provide them with evidence-based information about the benefits and risks of influenza vaccination. The nurse should also collaborate with the health department and other community partners to organize voluntary flu clinics that are accessible, affordable, and convenient for those who want to receive the vaccine.
Choice D reason: Closing the school for 6 weeks is not an appropriate action by the nurse, as it may not be necessary, practical, or beneficial in preventing influenza. Influenza outbreaks can vary in severity, duration, and impact depending on several factors, such as the strain of the virus, the level of immunity in the population, the availability of vaccines and antiviral medications, and the implementation of preventive measures. The nurse should monitor the situation closely and follow the guidance of the health authorities regarding school closure decisions. The nurse should also consider the potential consequences of school closure on the student's education, socialization, nutrition, safety, and mental health. The nurse should weigh the benefits and harms of school closure against other alternatives, such as increasing ventilation, cleaning and disinfecting surfaces, screening for symptoms, isolating sick students or staff members, reducing class size or mixing groups.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
Choice A reason: Proactive prevention is not a level of prevention, but rather a type of prevention that involves taking action before a problem occurs or worsens. It can be applied to any level of prevention, such as primary, secondary, or tertiary.
Choice B reason: Secondary prevention is a level of prevention that involves detecting and treating diseases or injuries early before they cause significant complications or disabilities. It includes activities such as screening tests, diagnostic tests, or medications.
Choice C reason: Tertiary prevention is a level of prevention that involves reducing the impact and consequences of diseases or injuries that have already occurred and caused damage or impairment. It includes activities such as rehabilitation, surgery, or palliative care.
Choice D reason: Primary prevention is a level of prevention that involves preventing diseases or injuries from occurring in the first place, by eliminating or reducing risk factors or enhancing protective factors. It includes activities such as immunization, education, or lifestyle modification. Advising a client with osteoporosis to have three servings of milk or dairy products daily is an example of primary prevention because it aims to prevent further bone loss and fractures by increasing calcium intake.
Correct Answer is B
Explanation
Choice A: Collaborate with a physical therapist to develop programs for injured employees to return to work. This is incorrect because this is a tertiary prevention strategy, not a secondary prevention strategy. Tertiary prevention aims to restore function and prevent disability or complications after an injury or illness has occurred.
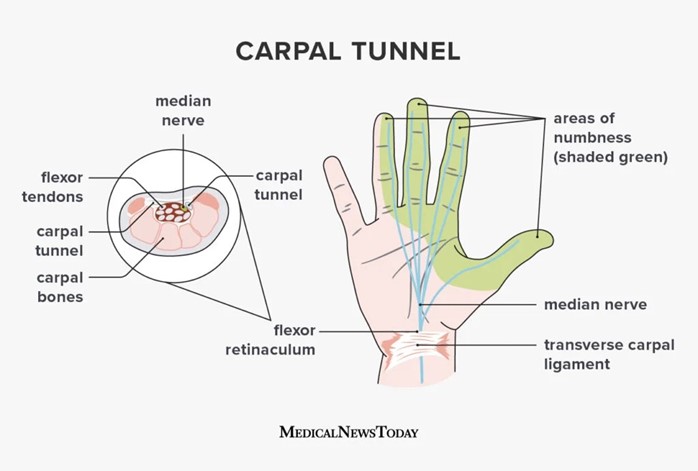
Choice B: Help plant workers identify signs of carpal tunnel syndrome. This is correct because this is a secondary prevention strategy. Secondary prevention aims to detect and treat health problems early before they become more serious or chronic. Carpal tunnel syndrome is a common occupational health problem that can cause pain, numbness, and weakness in the hand and wrist. Early identification and treatment can prevent permanent nerve damage and disability.
Choice C: Organize an influenza immunization campaign. This is incorrect because this is a primary prevention strategy, not a secondary prevention strategy. Primary prevention aims to prevent disease or injury from occurring in the first place, by reducing exposure or risk factors. Influenza immunization can protect plant workers from getting infected by the flu virus and reduce the spread of the disease.
Choice D: Teach plant workers about proper lifting techniques. This is incorrect because this is also a primary prevention strategy, not a secondary prevention strategy. Proper lifting techniques can prevent musculoskeletal injuries such as sprains, strains, and herniated discs, by avoiding excessive stress on the spine and joints.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
