Brain Tumors: Gliomas, Meningiomas, Metastatic brain tumors
- Brain tumors are abnormal growths of cells in the brain or surrounding tissues
- Brain tumors can be classified as primary or secondary, benign or malignant, and according to their location and cell type
- Primary brain tumors originate in the brain or its coverings (meninges), such as gliomas, meningiomas, pituitary adenomas, acoustic neuromas, etc.
- Secondary brain tumors (also called metastatic brain tumors) result from cancer cells that spread from another part of the body to the brain, such as lung cancer, breast cancer, melanoma, etc.
- Benign brain tumors are noncancerous and do not invade nearby tissues or spread to other parts of the body. However, they can still cause symptoms by compressing or displacing normal brain structures
- Malignant brain tumors are cancerous and can invade nearby tissues or spread to other parts of the body. They are more aggressive and have a poorer prognosis than benign brain tumors
- The location of a brain tumor determines its effects on the brain functions. For example, a tumor in the frontal lobe can affect personality, judgment, memory, etc., while a tumor in the temporal lobe can affect language, hearing, emotion, etc.
- The cell type of a brain tumor determines its characteristics and behavior. For example, gliomas are derived from glial cells and are graded from I to IV based on their degree of malignancy. Grade I gliomas are slow-growing and benign, while grade IV gliomas (glioblastoma multiforme) are fast-growing and highly malignant
- The nervous system consists of the central nervous system (CNS) and the peripheral nervous system (PNS). The CNS includes the brain and the spinal cord, while the PNS includes the nerves that connect the CNS to the rest of the body.
- The brain is composed of billions of neurons (nerve cells) that communicate with each other through electrical and chemical signals. The neurons are supported by glial cells, which provide structural and functional support, such as nutrition, metabolism, immunity, myelin formation, and synaptic modulation.
- A brain tumor is an abnormal mass of tissue that grows in or around the brain. Brain tumors can be primary (originating in the brain) or secondary (spreading from another part of the body). Primary brain tumors can be benign (non-cancerous) or malignant (cancerous).
- The nervous system is composed of the central nervous system (CNS), which includes the brain and spinal cord, and the peripheral nervous system (PNS), which includes the cranial and spinal nerves.
- The CNS is protected by three layers of membranes called meninges: the dura mater, the arachnoid mater, and the pia mater. The meninges also contain blood vessels and cerebrospinal fluid (CSF) that nourish and cushion the CNS.
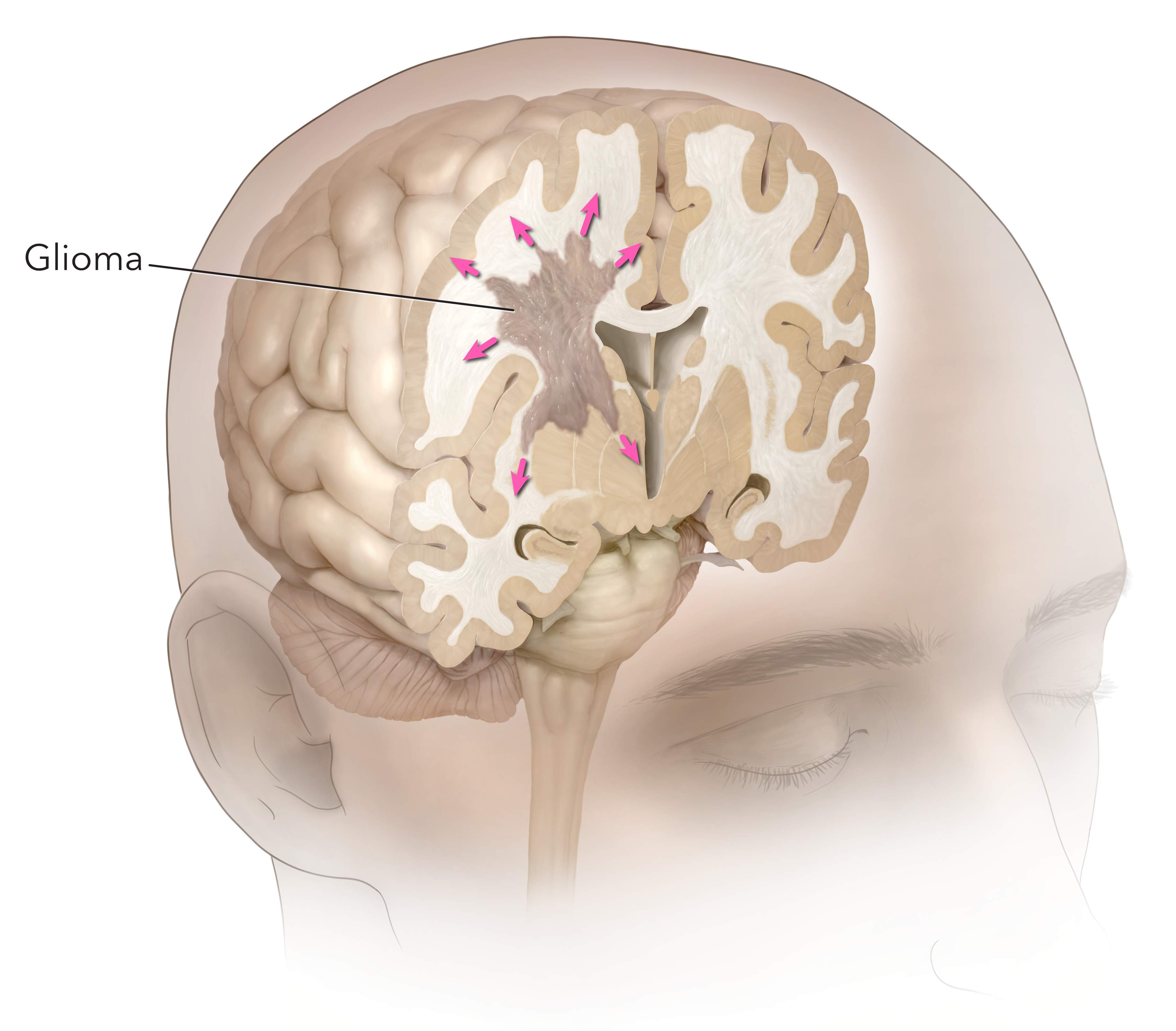
- A glioma is a tumor that originates from the glial cells in the brain or spinal cord. It is the most common type of primary brain tumor, accounting for about 30% of all brain tumors. Gliomas can affect children or adults, but are more common in older adults (over 65) and white people.
- Gliomas are classified into different types based on the type of glial cell they arise from: astrocytomas (from astrocytes), ependymomas (from ependymal cells), oligodendrogliomas (from oligodendrocytes), or mixed gliomas (from more than one type of glial cell).
- Gliomas are also graded according to their degree of malignancy (cancerousness), aggressiveness, and invasiveness. The World Health Organization (WHO) uses a four-tier grading system: grade I (low-grade or benign), grade II (low-grade or slow-growing), grade III (high-grade or anaplastic), and grade IV (high-grade or glioblastoma).
- Gliomas can cause various symptoms depending on their location, size, and growth rate. Some common symptoms include headache, nausea, vomiting, confusion, memory loss, personality changes, vision problems, speech difficulties, seizures, muscle weakness, and balance problems.
- Gliomas are diagnosed by a neurological examination, imaging tests (such as CT scan, MRI scan, PET scan), and biopsy (taking a sample of the tumor tissue for microscopic analysis).
- Gliomas are treated by a multidisciplinary team of specialists, such as neurologists, neurosurgeons, radiation oncologists, medical oncologists, nurses, and other allied health professionals. The treatment options include surgery (to remove as much of the tumor as possible), radiation therapy (to destroy the remaining tumor cells with high-energy beams), chemotherapy (to kill the tumor cells with drugs), targeted drug therapy (to block specific molecules or pathways that drive tumor growth), and supportive care (to manage symptoms and complications).
- Astrocytoma is the most common type of glioma. It arises from astrocytes, which are star-shaped cells that regulate the blood-brain barrier, the extracellular fluid, and neurotransmitter uptake. Astrocytomas can be low-grade (grade I or II) or high-grade (grade III or IV). Low-grade astrocytomas grow slowly and may not cause symptoms for years. High-grade astrocytomas grow rapidly and invade nearby tissues. The most aggressive form of astrocytoma is glioblastoma (grade IV), which has a poor prognosis (median survival of 15 months). A rare but very malignant form of astrocytoma that affects children is diffuse intrinsic pontine glioma (DIPG), which grows in the brain stem and causes cranial nerve dysfunction.
- Oligodendroglioma is a rare type of glioma that arises from oligodendrocytes, which are cells that produce myelin (a fatty substance that insulates the nerve fibers). Oligodendrogliomas tend to grow slowly and have a better prognosis than astrocytomas. They are usually low-grade (grade II) or anaplastic (grade III). Oligodendrogliomas often have genetic mutations that make them more sensitive to chemotherapy and radiation therapy. They are more common in adults than children and usually occur in the frontal or temporal lobes of the brain.
- Ependymoma is another rare type of glioma that arises from ependymal cells, which are cells that line the ventricles (fluid-filled spaces) of the brain and the central canal of the spinal cord. Ependymomas can be low-grade (grade I or II) or anaplastic (grade III). They can block the flow of cerebrospinal fluid (CSF), causing increased intracranial pressure (ICP) and hydrocephalus (water on the brain). Ependymomas can also spread through the CSF to other parts of the brain or spinal cord. They are more common in children than adults and usually occur in the posterior fossa (the back part of the skull) or the spinal cord.
- Gliomas can cause various complications and challenges for patients and their families. Some of these include:
- Seizures: Gliomas can irritate or damage the brain cells that control electrical activity, causing abnormal bursts of signals that result in seizures. Seizures can affect different parts of the body, such as the muscles, sensations, emotions, or consciousness. Seizures can be treated with anticonvulsant drugs, such as gabapentin or lamotrigine, but may have side effects such as drowsiness, dizziness, or rash.
- Cognitive impairment: Gliomas can affect the brain functions that are responsible for thinking, learning, memory, language, and behavior. Cognitive impairment can manifest as confusion, forgetfulness, difficulty concentrating, aphasia (loss of speech), dysarthria (slurred speech), or personality changes. Cognitive impairment can be assessed by neuropsychological tests and managed by cognitive rehabilitation, speech therapy, occupational therapy, or supportive devices.
- Recurrence: Gliomas can recur after treatment, either in the same location or in a different part of the brain or spinal cord. Recurrence can be detected by regular follow-up imaging tests and monitored by tumor markers, such as MGMT (a gene that predicts response to chemotherapy) or IDH1/2 (genes that indicate tumor grade and prognosis). Recurrence can be treated by repeat surgery, radiation therapy, chemotherapy, targeted drug therapy, or clinical trials.
- Quality of life: Gliomas can affect the physical, emotional, social, and spiritual aspects of a patient’s life. Quality of life can be measured by standardized questionnaires and improved by palliative care, which aims to relieve symptoms and enhance comfort. Quality of life can also be enhanced by psychosocial support, such as counseling, support groups, education, or complementary therapies.
- Nursing care for patients with gliomas involves applying the nursing process to plan and provide holistic care that meets the individual needs and preferences of each patient and their family. The nursing process consists of five steps: assessment, diagnosis, planning, implementation, and evaluation.
- Assessment: The nurse collects data about the patient’s health history, physical examination, diagnostic tests, symptoms, complications, medications, treatments, coping strategies, support systems, and goals. The nurse uses various tools and techniques to gather data, such as observation, interview, inspection, palpation, percussion, auscultation, or standardized scales.
- Diagnosis: The nurse analyzes the data and identifies the patient’s actual or potential health problems or needs. The nurse uses standardized terminology to formulate nursing diagnoses, which are statements that describe the patient’s response to their health condition. For example, a nursing diagnosis for a patient with glioma could be “Risk for ineffective cerebral tissue perfusion related to increased intracranial pressure”.
- Planning: The nurse prioritizes the patient’s nursing diagnoses and sets measurable and realistic goals and outcomes for each one. The nurse also selects appropriate nursing interventions that are evidence-based and consistent with the patient’s preferences and values. For example, a goal for a patient with glioma could be “The patient will maintain normal intracranial pressure within 24 hours” and an intervention could be “Monitor vital signs, neurological status, and ICP hourly”.
- Implementation: The nurse performs the planned interventions and documents their actions and outcomes. The nurse also coordinates care with other members of the healthcare team and involves the patient and family in decision making and education. An example of implementation could be “Administer anticonvulsant drugs as prescribed and observe for adverse effects”.
- Evaluation: The nurse evaluates the patient’s progress and outcomes and compares them with the expected goals and outcomes. The nurse also modifies the plan of care as needed based on the evaluation results and feedback from the patient and family. For example, an evaluation for a patient with glioma could be “The patient’s intracranial pressure was within normal range (10-15 mmHg) for 24 hours and the patient reported no headache, nausea, or vision problems”.
- A meningioma is a tumor that arises from the meningeal cells, usually in the dura mater. It is not technically a brain tumor, but it can compress or invade the adjacent brain tissue, nerves, or vessels, causing various neurological symptoms.
- Meningiomas are the most common type of primary CNS tumor, accounting for about one-third of all cases. They occur more frequently in middle-aged women, but they can affect anyone at any age.
- Meningiomas are classified into three grades based on their histological features and biological behavior: grade I (benign), grade II (atypical), and grade III (malignant). Each grade includes different subtypes that have different molecular markers and prognoses.
- The exact cause of meningiomas is unknown, but some possible factors include:
- Exposure to ionizing radiation, especially in childhood or during radiation therapy for other conditions.
- Genetic mutations or disorders, such as neurofibromatosis type 2 (NF2), which is associated with bilateral vestibular schwannomas and multiple meningiomas.
- Hormonal influences, such as estrogen receptors found in some meningiomas, which may explain the higher incidence in women. Some studies suggest that oral contraceptives or hormone replacement therapy may increase the risk of meningioma growth.
- Other factors, such as obesity, head trauma, infection, or inflammation, which may contribute to meningioma development or progression.
- The signs and symptoms of meningiomas depend on their location, size, grade, and rate of growth. Some common manifestations include:
- Headache, which is often worse in the morning or with changes in position. It may be caused by increased intracranial pressure (ICP), mass effect, or irritation of pain-sensitive structures.
- Seizures, which may be focal or generalized. They may result from compression or invasion of cortical areas or epileptogenic foci.
- Visual disturbances, such as blurred vision, diplopia (double vision), hemianopia (loss of half of the visual field), or papilledema (swelling of the optic disc). They may occur due to compression or invasion of the optic nerve, chiasm, tract, or radiation.
- Hearing loss or tinnitus (ringing in the ears), which may be caused by compression or invasion of the acoustic nerve or vestibulocochlear nerve.
- Cranial nerve palsies, which may affect any of the 12 cranial nerves and cause various sensory or motor deficits. For example, facial weakness or numbness may result from compression or invasion of the facial nerve or trigeminal nerve.
- Cognitive impairment or personality changes, which may be due to compression or invasion of frontal lobes, temporal lobes, or other areas involved in memory, language, judgment, or behavior.
- Motor weakness or sensory loss, which may affect one or more limbs depending on the location of the tumor. It may be caused by compression or invasion of motor cortex, corticospinal tract, or spinal cord.
- The diagnosis of meningiomas is based on a combination of clinical history, physical examination, neurological assessment, and imaging studies. Some common tests and procedures include:
- Magnetic resonance imaging (MRI), which is the preferred modality for detecting and characterizing meningiomas. It can provide detailed information about the tumor size, shape, location, enhancement pattern, edema, mass effect, and invasion. It can also help differentiate between different subtypes of meningiomas based on their signal intensity and contrast uptake.
- Computed tomography (CT) scan, which can also show the presence and features of meningiomas, but with less resolution and contrast than MRI. It can be useful for detecting calcifications, bone erosion, or hyperostosis (thickening of the skull) associated with some meningiomas.
- Angiography, which can show the blood supply and vascularization of meningiomas. It can help plan for surgical resection or embolization of the tumor.
- Lumbar puncture, which can measure the CSF pressure and analyze the CSF composition. It can help rule out other causes of increased ICP, such as infection or hemorrhage. It can also detect tumor cells or markers in the CSF in some cases of malignant meningiomas.
- Biopsy, which is the definitive method for confirming and grading meningiomas. It involves taking a small sample of tumor tissue and examining it under a microscope. It can also help identify the molecular markers and genetic alterations of the tumor, which can guide the treatment and prognosis.
- The treatment of meningiomas depends on several factors, such as the tumor grade, size, location, symptoms, and patient preferences. Some common options include:
- Surgery, which is the mainstay of treatment for most meningiomas. The goal is to achieve a gross total resection (GTR), which means removing the entire tumor and its attachments to the dura mater. This can improve the symptoms, reduce the recurrence rate, and prolong the survival. However, surgery may not be possible or advisable in some cases, such as when the tumor is located in an inaccessible or eloquent area (such as the brainstem or optic nerve), or when the patient has significant comorbidities or risks. In these cases, a subtotal resection (STR) or a biopsy may be performed instead.
- Radiation therapy, which involves delivering high-energy rays to the tumor site to destroy the tumor cells or prevent their growth. It can be used as an adjuvant therapy after surgery to reduce the recurrence rate, especially for grade II or III meningiomas or for residual tumors after STR. It can also be used as a primary therapy for inoperable or recurrent meningiomas, or as a palliative therapy for symptomatic relief. There are different types of radiation therapy, such as external beam radiation therapy (EBRT), stereotactic radiosurgery (SRS), or brachytherapy.
- Pharmacological management, which involves using medications to treat the symptoms or slow down the growth of meningiomas. There are no specific drugs approved for meningiomas, but some agents that have been used in clinical trials or off-label include corticosteroids (to reduce edema and ICP), anticonvulsants (to prevent seizures), analgesics (to relieve pain), antiangiogenic drugs (to inhibit blood vessel formation), hormonal drugs (to block estrogen receptors), and chemotherapeutic drugs (to kill tumor cells).
- The nursing interventions for meningiomas are aimed at providing holistic care to the patient and family throughout the course of the disease. Some common interventions include:
- Assessing and monitoring the patient’s neurological status, vital signs, ICP, pain level, and response to treatment. Reporting any changes or abnormalities to the health care provider promptly.
- Administering medications as prescribed and monitoring their effects and side effects. Educating the patient and family about the purpose, dosage, route, frequency, and potential interactions of each drug.
- Preparing the patient for surgery or radiation therapy and providing postoperative or post-treatment care. Following the standard precautions and protocols for infection control, wound care, fluid and electrolyte balance, nutrition support, mobility assistance, and complication prevention.
- Providing emotional support and counseling to the patient and family. Addressing their fears, concerns, expectations, and coping strategies. Referring them to appropriate resources or services if needed.
- Educating the patient and family about the disease process, treatment options, prognosis, and follow-up care. Encouraging them to participate in decision making and self-care activities. Providing them with written instructions and contact information.
- The complications and outcomes of meningiomas vary depending on several factors, such as the tumor grade, size, location, treatment modality, and patient characteristics. Some possible complications include:
- Recurrence or progression of the tumor, which may require repeated surgery or radiation therapy. The recurrence rate is higher for grade II or III meningiomas, or for tumors that are incompletely resected.
- Neurological deficits, which may result from compression or invasion of brain tissue, nerves, or vessels by the tumor or its treatment. They may affect vision, hearing, speech, cognition, motor function, sensory function, or cranial nerve function. Some deficits may be temporary or reversible, while others may be permanent or progressive.
- Increased ICP, which may cause headache, nausea, vomiting, drowsiness, confusion, or coma. It may result from tumor growth, edema, hemorrhage, hydrocephalus, or infection. It may require urgent intervention to prevent brain herniation or death.
- Infection, which may occur at the surgical site, in the CSF, or in the bloodstream. It may cause fever, chills, malaise, wound drainage, meningitis, or sepsis. It may require antibiotic therapy and wound care.
- Hemorrhage, which may occur during or after surgery or radiation therapy. It may cause bleeding in the brain tissue, subdural space, epidural space, or subarachnoid space. It may cause increased ICP, stroke-like symptoms, or death.
- Radiation-induced injury, which may occur after radiation therapy. It may cause delayed effects such as radiation necrosis (tissue death), vasculopathy (blood vessel damage), leukoencephalopathy (white matter damage), or secondary tumors. It may cause neurological deterioration or cognitive decline.
- The outcomes of meningiomas depend on the tumor grade and the extent of resection. The survival rates are generally high for grade I meningiomas (>90% at 10 years), intermediate for grade II meningiomas (50-80% at 10 years), and low for grade III meningiomas (10-30% at 10 years). The quality of life is also affected by the presence and severity of neurological deficits and complications.
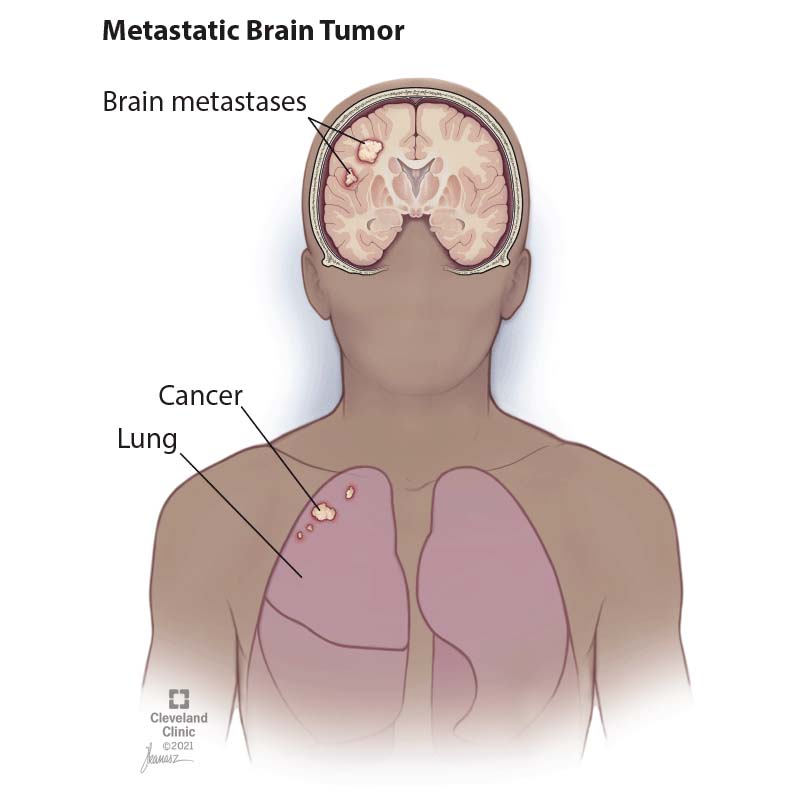
- Metastatic brain tumors are more common than primary brain tumors. They account for about 40% of all intracranial neoplasms1
- Metastatic brain tumors usually occur in multiple sites within the brain. The most common locations are the cerebral hemispheres (80%), cerebellum (15%), and brainstem (5%)2
- Metastatic brain tumors usually arise from cancers that have a high propensity to spread to the brain via hematogenous or lymphatic routes. The most common primary cancers that cause metastatic brain tumors are lung cancer (50%), breast cancer (15%), melanoma (10%), renal cell carcinoma (5%), and colorectal cancer (5%)3
- Metastatic brain tumors can cause symptoms by increasing intracranial pressure (ICP), causing cerebral edema (swelling), hemorrhage (bleeding), or hydrocephalus (accumulation of cerebrospinal fluid), or by affecting specific functions of the affected regions of the brain
- The symptoms of metastatic brain tumors depend on their size, number, location, rate of growth, and response to treatment. The most common symptoms are headache (50%), seizures (30%), focal neurological deficits (25%), cognitive impairment (20%), nausea/vomiting (15%), papilledema (10%), and personality changes (10%)4
- The diagnosis of brain tumors and metastatic brain tumors is based on a combination of clinical history, physical examination, neurological examination, imaging studies, laboratory tests, and biopsy
- Clinical history: The patient’s medical history, family history, risk factors, symptoms, duration, frequency, severity, and triggers are obtained to assess the possibility of a brain tumor
- Physical examination: The patient’s vital signs, general appearance, skin condition, head/neck examination, eye examination, ear/nose/throat examination, cardiovascular examination, respiratory examination, abdominal examination, musculoskeletal examination, and neurological examination are performed to evaluate the patient’s overall health status and detect any signs of increased ICP, focal neurological deficits, or systemic diseases
- Neurological examination: The patient’s mental status, cranial nerve functions, motor functions, sensory functions, coordination, reflexes, and gait are assessed to determine the location and extent of the brain tumor
- Imaging studies: The most commonly used imaging modalities for brain tumors and metastatic brain tumors are computed tomography (CT) scan and magnetic resonance imaging (MRI) scan. These tests can provide detailed information about the size, shape, location, number, and characteristics of the brain tumor and its effects on the surrounding structures. Other imaging tests that may be used are positron emission tomography (PET) scan, single-photon emission computed tomography (SPECT) scan, magnetic resonance spectroscopy (MRS), and magnetic resonance angiography (MRA)
- Laboratory tests: The patient’s blood, urine, cerebrospinal fluid (CSF), and tumor tissue samples may be analyzed to detect any abnormalities in the levels of glucose, electrolytes, blood cells, hormones, tumor markers, genetic mutations, etc. that may indicate the presence or type of brain tumor
- Biopsy: The definitive diagnosis of a brain tumor or a metastatic brain tumor requires a biopsy, which is the removal of a small sample of the tumor tissue for microscopic examination. A biopsy can confirm the type and grade of the tumor and guide the treatment plan. A biopsy can be performed by surgery (open or stereotactic) or by needle aspiration (fine-needle or core-needle)
- The treatment of brain tumors and metastatic brain tumors depends on several factors, such as the type, grade, size, location, number, and symptoms of the tumor; the patient’s age, general health, preferences, and goals; and the availability and effectiveness of the treatment modalities
- The main treatment options for brain tumors and metastatic brain tumors are surgery, radiation therapy, chemotherapy, immunotherapy, targeted therapy, and palliative care
- Surgery: Surgery is the preferred treatment for most brain tumors and some metastatic brain tumors that are accessible and resectable. Surgery aims to remove as much of the tumor as possible while preserving the normal brain function. Surgery can also reduce the mass effect of the tumor and relieve the symptoms of increased ICP. Surgery can be performed by craniotomy (opening of the skull) or by minimally invasive techniques (endoscopy or laser ablation). Surgery may be combined with other treatments such as radiation therapy or chemotherapy
- Radiation therapy: Radiation therapy uses high-energy rays or particles to kill cancer cells or stop their growth. Radiation therapy can be used as a primary treatment for some brain tumors and metastatic brain tumors that are inoperable or incompletely resected. Radiation therapy can also be used as an adjuvant treatment after surgery to prevent recurrence or as a palliative treatment to relieve symptoms. Radiation therapy can be delivered by external beam radiation therapy (EBRT), stereotactic radiosurgery (SRS), brachytherapy (implantation of radioactive seeds), or radioisotope therapy (injection of radioactive substances)
- Chemotherapy: Chemotherapy uses drugs to kill cancer cells or stop their growth. Chemotherapy can be used as a primary treatment for some brain tumors and metastatic brain tumors that are sensitive to drugs. Chemotherapy can also be used as an adjuvant treatment after surgery or radiation therapy to prevent recurrence or as a palliative treatment to relieve symptoms. Chemotherapy can be administered by oral route, intravenous route, intrathecal route (injection into the CSF), or intra-arterial route (injection into the blood vessel supplying the tumor). Chemotherapy may be combined with other treatments such as radiation therapy or targeted therapy
- Immunotherapy: Immunotherapy uses substances that stimulate or modify the immune system to fight cancer cells. Immunotherapy can be used as a primary treatment for some brain tumors and metastatic brain tumors that express specific antigens or receptors. Immunotherapy can also be used as an adjuvant treatment after surgery or radiation therapy to prevent recurrence or as a palliative treatment to relieve symptoms. Immunotherapy can be administered by intravenous route, subcutaneous route, intratumoral route (injection into the tumor), or intraventricular route (injection into the ventricles of the brain). Immunotherapy may include monoclonal antibodies, cytokines, vaccines, or adoptive cell transfer
- Targeted therapy: Targeted therapy uses drugs that target specific molecules or pathways involved in the growth and survival of cancer cells. Targeted therapy can be used as a primary treatment for some brain tumors and metastatic brain tumors that have specific genetic mutations or alterations. Targeted therapy can also be used as an adjuvant treatment after surgery or radiation therapy to prevent recurrence or as a palliative treatment to relieve symptoms. Targeted therapy can be administered by oral route, intravenous route, or intra-arterial route (injection into the blood vessel supplying the tumor). Targeted therapy may include tyrosine kinase inhibitors, angiogenesis inhibitors, or proteasome inhibitors
- Palliative care is a holistic approach that aims to improve the quality of life of patients and their families who are facing life-threatening illnesses such as brain tumors and metastatic brain tumors
- Palliative care focuses on relieving the physical, emotional, social, and spiritual suffering of patients and their families
- Palliative care can be provided at any stage of the disease, along with other treatments or as the main treatment when no cure is possible
- Palliative care can be delivered by a multidisciplinary team of health professionals, such as physicians, nurses, social workers, psychologists, chaplains, etc.
- Palliative care can involve various interventions, such as pain management, symptom control, psychosocial support, spiritual care, advance care planning, hospice care, and bereavement care
- Brain tumors and metastatic brain tumors can cause various complications that can affect the patient’s survival and quality of life
- The most common complications are increased ICP, cerebral herniation, brainstem compression, hydrocephalus, seizures, hemorrhage, infection, neurological deficits, cognitive impairment, behavioral changes, endocrine disorders, and systemic effects
- The prognosis of brain tumors and metastatic brain tumors depends on several factors, such as the type, grade, size, location, number, and symptoms of the tumor; the patient’s age, general health, preferences, and goals; and the availability and effectiveness of the treatment modalities
- The prognosis of brain tumors and metastatic brain tumors is usually poor. The median survival time for primary brain tumors ranges from 1 to 15 years, depending on the type and grade of the tumor. The median survival time for metastatic brain tumors is about 6 months
Gliomas
Complications and Challenges
Nursing Care
Meningiomas

Nursing Interventions
Complications and Outcomes
Metastatic Brain Tumors
Diagnostic Tests and Procedures
Treatment Options and Nursing Interventions
Palliative Care
Complications and Prognosis
Nursing Test Bank
Test Bank #1: RN Pharmacology Exams
Test Bank #2: RN Medical-Surgical Exams
Test Bank #3: RN Fundamentals Exams
Test Bank #4: RN Maternal-Newborn Exams
Test Bank #5: RN Anatomy and Physiology Exams
Test Bank #6: RN Obstetrics and Pediatrics Exams
Test Bank #7: RN Fluid and Electrolytes Exams
Test Bank #9: RN Adult Health
Test Bank #10: RN Dosage Calculation
Test Bank #11: RN Community Health Exams
Test Bank #12: RN Psychology Exams
Test Bank #13: RN Nursing Care Of Children
Test Bank #14: RN Foundations of Nursing Exams
Naxlex Comprehensive Predictor Exams
Exam #1: RN Comprehensive predictor 2023 proctored exam
Exam #2: Ati rn vati comprehensive predictor proctored exam
Exam #3: Ati Rn Comprehensive Predictor Proctored Exam 2023
Exam #4: Rn Comprehensive Predictor 2023 Proctored Exam - St. Joseph
Exam #5: RN Comprehensive Predictor Proctored Exam (National U CA San Diego)
Exam #6: Ati rn comprehensive predictor 2023 retake proctored exam
Exam #7: RN Hesi Exit Proctored Exam
Exam #8: Hesi RN Exit proctored exam
Exam #9: Hesi rn exit proctored exam
Exam #10: Hesi Rn compass exit B proctored exam
Questions on Brain Tumors: Gliomas, Meningiomas, Metastatic brain tumors
Correct Answer is C
Explanation
This statement is not indicative of a meningioma, but of a supratentorial tumor, which occurs in the cerebral hemispheres above the tentorium cerebelli and may cause loss of voluntary movement or hemiparesis (weakness or numbness on one side of the body).
Correct Answer is B
Explanation
Acoustic nerve cells are not the origin of gliomas, but of acoustic neuromas, which are benign brain tumors that arise from the acoustic cranial nerve and may cause hearing loss or ringing in the ears.
Correct Answer is A
Explanation
This statement is not an adverse effect of chemotherapy, but of the brain tumor itself. Brain tumors can cause seizures by affecting the function of different areas of the brain and disrupting the electrical activity of neurons.
Correct Answer is ["A","B","C","E"]
Explanation
This statement is true. Metastatic brain tumors can cause increased intracranial pressure and neurological deficits by applying pressure to surrounding brain tissue and impairing cerebral blood flow and cerebrospinal fluid drainage.
This statement is false. Hemiparesis is weakness or paralysis of one side of the body that can affect the face, arm, or leg. It is caused by damage to the cerebral cortex or the corticospinal tract, which control voluntary movement.
This statement is false. Skin erythema at the radiation site is not a sign of radiation necrosis, but a common side effect of radiation therapy that occurs when skin cells are damaged by radiation exposure. Skin erythema at the radiation site is usually mild and self-limiting.
This statement is not specific to the surgery, but to the location of the brain tumor. Brain tumors that involve the cranial nerves can cause hearing loss, vision loss, or facial paralysis by impairing their function.
This statement is not correct. Acoustic neuromas are benign brain tumors that arise from the acoustic cranial nerve and may cause hearing loss or ringing in the ears, vertigo, facial drooping, or difficulty swallowing, but they do not typically affect vision or reading ability.
Search Here
More on Nursing
- Pathophysiology of the Musculoskeletal System
- Pathophysiology of the Reproductive System
- Pathophysiology of the integumentary system
- Pathophysiology of the Hematologic System
- Pathophysiology of the respiratory system
- Pathophysiology of the renal system
- Pathophysiology of the Gastrointestinal System
- Basic Concepts of Pathophysiology
Free Nursing Study Materials
Access to all study guides and practice questions for nursing for free.
- Free Nursing Study Trials
- Free Nursing Video tutorials
- Free Nursing Practice Tests
- Free Exam and Study Modes
- Free Nursing Revision Quizlets
