Epilepsy and Seizure Disorders: Status epilepticus
- Epilepsy is a chronic neurological disorder that affects the brain. It is characterized by recurrent unprovoked seizures that result from abnormal synchronous electrical activity of a group of neurons in the brain
- Seizures are transient episodes of altered consciousness, behavior, sensation, motor activity, or autonomic function that result from abnormal electrical activity of a group of neurons in the brain
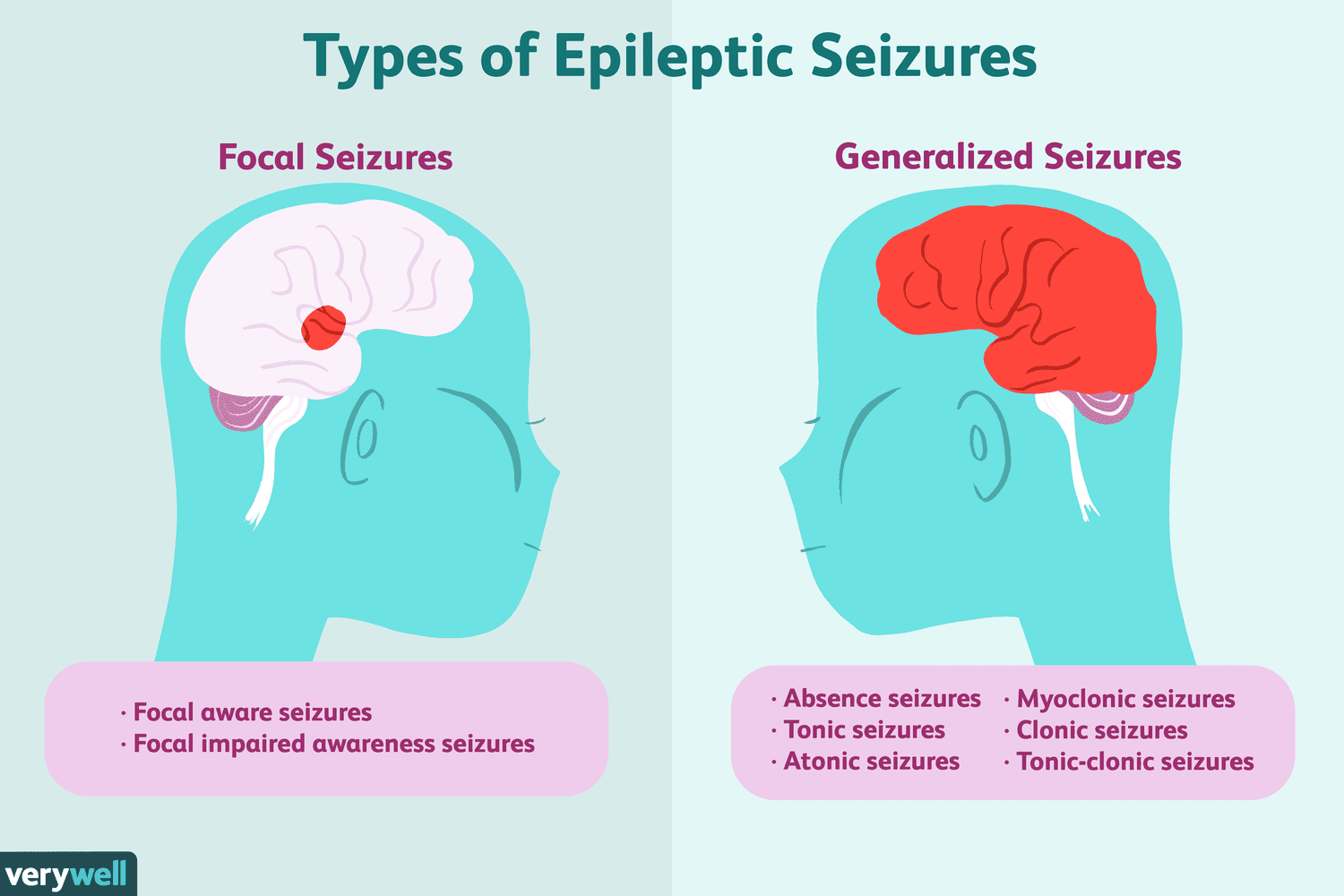
- Seizures can be classified into two main types: focal (partial) seizures and generalized seizures
- Focal seizures: Seizures that originate from a specific region of the brain and affect only one hemisphere. They can be further divided into:
- Focal aware seizures: Seizures that do not impair consciousness or awareness. They may cause motor symptoms (e.g., twitching, jerking, stiffening), sensory symptoms (e.g., tingling, numbness, flashing lights), autonomic symptoms (e.g., sweating, flushing, palpitations), or psychic symptoms (e.g., deja vu, fear, joy)
- Focal impaired awareness seizures: Seizures that impair consciousness or awareness. They may cause automatisms (e.g., lip smacking, fumbling, wandering), confusion, amnesia, or postictal (after seizure) symptoms (e.g., headache, fatigue, weakness)
- Generalized seizures: Seizures that involve both hemispheres of the brain and affect the whole body. They can be further divided into:
- Absence seizures: Seizures that cause brief lapses of consciousness or awareness. They may cause staring, blinking, or subtle movements
- Myoclonic seizures: Seizures that cause sudden brief muscle contractions or jerks. They may affect one or more limbs or the whole body
- Atonic seizures: Seizures that cause sudden loss of muscle tone or strength. They may cause falls or head drops
- Tonic seizures: Seizures that cause sudden increase of muscle tone or stiffness. They may cause rigid posture or extension of limbs
- Clonic seizures: Seizures that cause rhythmic muscle contractions or spasms. They may affect one or more limbs or the whole body
- Tonic-clonic seizures: Seizures that cause a combination of tonic and clonic phases. They may cause loss of consciousness, convulsions, biting of tongue, incontinence, etc.
- Focal seizures: Seizures that originate from a specific region of the brain and affect only one hemisphere. They can be further divided into:
- The causes of epilepsy and seizure disorders vary depending on the type and origin of the seizures.
- some common causes include
- genetic factors (e.g., mutations or syndromes),
- structural factors (e.g., trauma, stroke, tumor, infection),
- metabolic factors (e.g., electrolyte imbalance, hypoglycemia, hypoxia),
- immune factors (e.g., autoimmune diseases, inflammation),
- pharmacological factors (e.g., drug withdrawal, drug toxicity),
- idiopathic factors (e.g., unknown causes)
- Some factors that may increase the risk of developing epilepsy and seizure disorders include
- age (infants and older adults),
- sex (male),
- family history,
- head injury,
- brain infection (e.g., meningitis, encephalitis),
- brain tumor,
- stroke,
- dementia, etc.
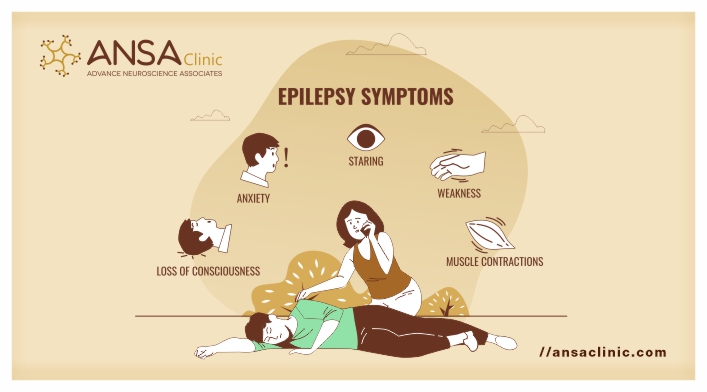
- The signs and symptoms of epilepsy and seizure disorders vary depending on the type and severity of the seizures.
- Some common manifestations include
- altered consciousness, behavior, sensation, motor activity, or autonomic function as described above;
- aura (a warning sign before a seizure such as a smell, sound, or feeling);
- prodrome (a mood or physical change before a seizure such as irritability, anxiety, or headache);
- postictal state (a recovery period after a seizure such as confusion, drowsiness, or weakness);
- status epilepticus (a prolonged or recurrent seizure that lasts more than 5 minutes or does not stop without treatment)
- The diagnosis of epilepsy and seizure disorders is based on clinical criteria that include medical history, physical examination, neurological examination, and exclusion of other possible causes.
- Some diagnostic tests that may be used to confirm the diagnosis or identify the type and origin of the seizures include:
- Electroencephalography (EEG): To measure the electrical activity of the brain using electrodes attached to the scalp that may show abnormal patterns or spikes that indicate seizure activity
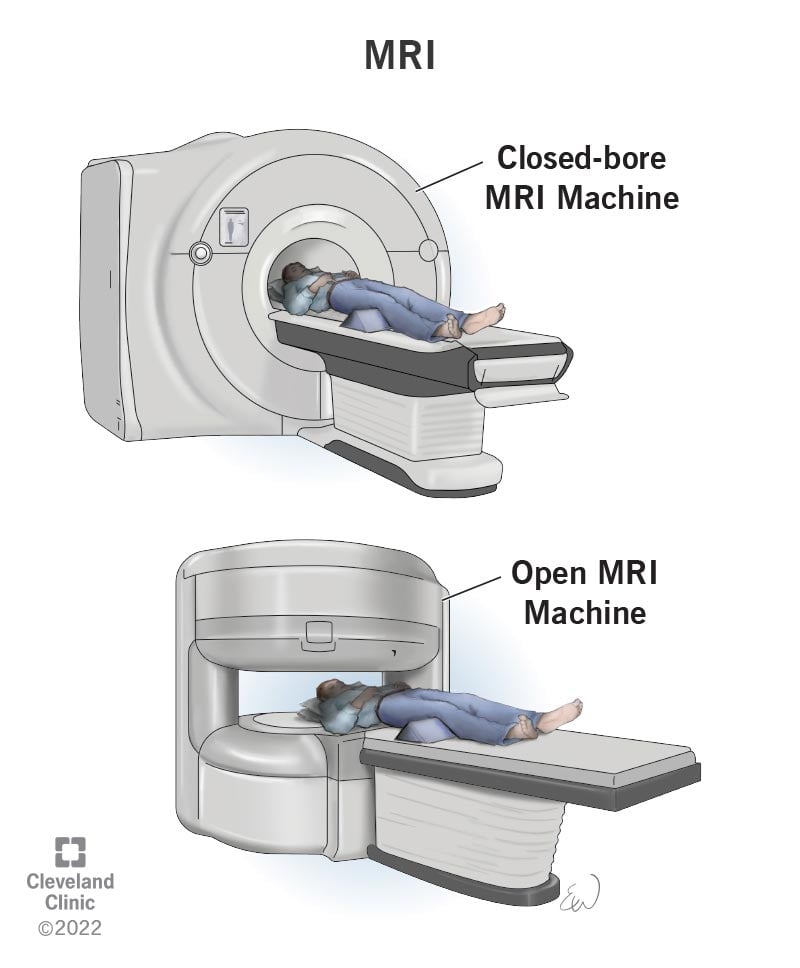
- Neuroimaging: To visualize the structure and function of the brain using techniques such as CT, MRI, PET, SPECT, etc. that may show structural abnormalities or lesions that cause seizures
- Blood tests: To check for metabolic disorders, infection, inflammation, drug levels, etc. that may cause or mimic seizures
- Lumbar puncture: To obtain a sample of CSF for analysis and culture that may show infection, inflammation, or bleeding that cause seizures
- The treatment of epilepsy and seizure disorders is aimed at controlling the seizures, reducing the side effects, improving the quality of life, and providing support and education for the patient and caregivers.
- Some treatment options include:
- Antiepileptic drugs (AEDs): To prevent or reduce the frequency and severity of seizures using drugs such as phenytoin, carbamazepine, valproic acid, lamotrigine, levetiracetam, etc. that act on various neurotransmitter systems or receptors to stabilize the electrical activity of the brain. These drugs may have side effects such as drowsiness, dizziness, rash, liver toxicity, etc.
- Surgery: To remove or disconnect the brain tissue that causes seizures using procedures such as lobectomy (removal of a lobe of the brain), hemispherectomy (removal of a hemisphere of the brain), corpus callosotomy (cutting of the corpus callosum that connects the two hemispheres of the brain), etc. These procedures may have risks such as infection, bleeding, stroke, cognitive impairment, etc.
- Neuromodulation: To stimulate or inhibit specific brain regions or nerves using devices such as vagus nerve stimulator (VNS), responsive neurostimulation (RNS), deep brain stimulation (DBS), transcranial magnetic stimulation (TMS), etc. that deliver electrical currents or magnetic fields to modulate neuronal activity. These devices may have side effects such as infection, bleeding, headache, voice changes, etc.
- Dietary therapy: To modify the intake of carbohydrates, fats, and proteins using diets such as ketogenic diet, modified Atkins diet, low glycemic index treatment, etc. that induce ketosis (a metabolic state that uses fat as the main source of energy) that may reduce seizure activity. These diets may have side effects such as weight loss, constipation, kidney stones, etc.
- Lifestyle therapy: To avoid or reduce triggers or factors that may provoke seizures using interventions such as stress management, sleep hygiene, exercise, etc. that involve coping with stress, getting enough sleep, performing physical activities, etc. These interventions may improve mood, energy, and well-being in epilepsy and seizure disorder patients
- The prevention of epilepsy and seizure disorders depends on the type and cause of the seizures.
- Some preventive measures include:
-
- avoiding head injury, infection, stroke, tumor, etc. that may damage the brain
- avoiding drugs, alcohol, caffeine, etc. that may alter the brain chemistry
- avoiding flashing lights, loud noises, etc. that may stimulate the brain
- taking AEDs as prescribed
- following a healthy lifestyle
- seeking medical attention if experiencing any signs or symptoms of seizures
- The nervous system consists of the central nervous system (CNS) and the peripheral nervous system (PNS)
- The CNS includes the brain and the spinal cord, which are responsible for processing and integrating sensory and motor information
- The PNS includes the cranial and spinal nerves, which connect the CNS to the rest of the body
- The nervous system communicates through electrical impulses and chemical signals called neurotransmitters
- A seizure is a sudden, abnormal, and excessive discharge of neurons in the brain that causes a change in behavior, sensation, or consciousness
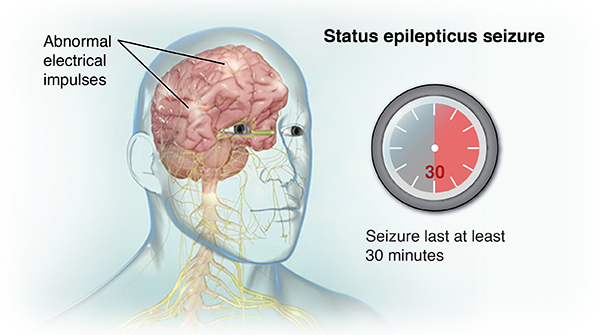
- Status epilepticus (SE) is a neurologic emergency that occurs when a seizure lasts longer than 5 minutes or when seizures occur very close together without recovery between them
- SE can be classified into two main types: generalized convulsive SE (GCSE) and nonconvulsive SE (NCSE)
- GCSE is characterized by repeated tonic-clonic seizures that involve both hemispheres of the brain and cause loss of consciousness, muscle contractions, and rhythmic jerking of the extremities
- NCSE is characterized by continuous or fluctuating altered mental status or behavior without overt motor manifestations
- SE can cause permanent brain damage or death if not treated promptly and effectively
- SE can be caused by various factors that trigger or exacerbate seizures, such as:
- Acute or chronic CNS disorders, such as stroke, trauma, infection, tumor, malformation, degeneration, or inflammation
- Metabolic disturbances, such as hypoglycemia, hyponatremia, hypocalcemia, hypomagnesemia, uremia, hepatic encephalopathy, or acidosis
- Drug toxicity or withdrawal, such as from alcohol, benzodiazepines, barbiturates, opioids, anticonvulsants, or illicit substances
- Acute or chronic systemic illnesses, such as sepsis, fever, hypoxia, hypotension, anemia, or electrolyte imbalance
- Genetic or idiopathic epilepsy syndromes, such as Dravet syndrome, Lennox-Gastaut syndrome, or febrile seizures
- The risk factors for SE vary depending on the age group and the underlying etiology of seizures
- In general, some risk factors include:
- History of epilepsy or previous seizures
- Nonadherence or subtherapeutic levels of anticonvulsant therapy
- African American race
- Male gender
- Low socioeconomic status
- Comorbidities that affect the CNS or metabolism
- SE occurs when the normal mechanisms that terminate a seizure fail to function properly
- This results in a mismatch of excitatory and inhibitory neurotransmitters in the brain, such as glutamate and gamma-aminobutyric acid (GABA)
- Glutamate is the main excitatory neurotransmitter that stimulates neuronal activity and increases calcium influx into neurons
- GABA is the main inhibitory neurotransmitter that reduces neuronal activity and increases chloride influx into neurons
- In SE, there is an excessive release of glutamate and a reduced release of GABA, leading to neuronal hyperexcitability and hypersynchronization
- SE can be divided into two phases: phase I and phase II
- Phase I occurs in the first 30 minutes of seizure activity and is characterized by increased autonomic activity and cerebral blood flow
- Each seizure causes a sharp increase in epinephrine, norepinephrine, and steroid concentrations that cause hypertension, tachycardia, cardiac arrhythmias, hyperglycemia, hyperthermia, sweating, and salivation
- Cerebral blood flow is increased to meet the increased metabolic demand of the brain during seizures
- Increased sympathetic and parasympathetic stimulation with muscle hypoxia can lead to ventricular arrhythmias, severe acidosis, and rhabdomyolysis (breakdown of muscle tissue)
- Shock, hypotension, hyperkalemia, and acute tubular necrosis may occur as a result of prolonged muscle contractions and tissue damage
- Phase II occurs after 30 minutes of seizure activity and is characterized by loss of cerebral autoregulation, decreased cerebral blood flow, increased intracranial pressure, and systemic hypotension
- The body is no longer able to compensate for the increased metabolic demand of the brain and the seizures become self-sustaining
- Hypoglycemia, hyperthermia, respiratory failure, hypoxia, respiratory and metabolic acidosis, hyperkalemia, hyponatremia, and uremia may develop as a result of impaired organ function and homeostasis
- The prolonged and recurrent seizures can cause neuronal injury and death through various mechanisms, such as:
- Excitotoxicity, which is the excessive stimulation of neurons by glutamate that leads to calcium overload and oxidative stress
- Apoptosis, which is the programmed cell death that is triggered by mitochondrial dysfunction and DNA damage
- Necrosis, which is the uncontrolled cell death that is caused by energy depletion and membrane disruption
- Inflammation, which is the activation of immune cells and cytokines that cause further neuronal damage and edema
- The neuronal injury and death can result in permanent brain damage or death, depending on the extent and location of the affected brain regions
- The clinical manifestations of SE depend on the type, duration, and severity of seizures, as well as the underlying etiology and comorbidities of the patient
- In general, some common signs and symptoms include:
- Altered level of consciousness, ranging from confusion to coma
- Motor manifestations, such as tonic-clonic movements, myoclonus, focal seizures, or subtle twitching
- Autonomic manifestations, such as hypertension, tachycardia, cardiac arrhythmias, hyperthermia, sweating, salivation, or incontinence
- Neurologic manifestations, such as headache, visual disturbances, aphasia, hemiparesis, or focal deficits
- Metabolic manifestations, such as hypoglycemia, hyponatremia, hyperkalemia, acidosis, or uremia
- Respiratory manifestations, such as hypoxia, hypercapnia, respiratory failure, or pulmonary edema
- Musculoskeletal manifestations, such as rhabdomyolysis, muscle breakdown, or compartment syndrome
- The diagnosis of SE is based on the clinical history and presentation of the patient, as well as the results of laboratory and imaging tests
- The diagnosis requires a high index of suspicion and prompt recognition of seizure activity and its duration
- The diagnosis can be confirmed by electroencephalography (EEG), which is the gold standard for detecting seizure activity in the brain
- EEG can also help to differentiate between GCSE and NCSE, as well as to identify the seizure focus and etiology
- EEG should be performed as soon as possible after the onset of SE or after the administration of initial anticonvulsant therapy
- Other diagnostic tests that may be performed include:
- Blood tests to measure glucose, electrolytes, calcium, magnesium, liver function tests, renal function tests, blood cultures, arterial blood gas, and serum anticonvulsant levels
- Urine tests to screen for drugs or toxins that may cause or worsen seizures
- Lumbar puncture to obtain cerebrospinal fluid (CSF) for analysis and culture to rule out CNS infection or inflammation
- Computed tomography (CT) scan or magnetic resonance imaging (MRI) of the brain to detect structural lesions or abnormalities that may cause or result from seizures
- The treatment of SE aims to stop the seizures as quickly and safely as possible, to identify and treat the underlying cause, and to prevent complications and recurrence
- The treatment involves a stepwise approach that consists of three stages: initial stabilization, initial therapy, and refractory therapy
- Initial stabilization involves securing the airway, breathing, and circulation (ABCs) of the patient, as well as monitoring vital signs, oxygen saturation, and glucose levels
- Initial therapy involves administering intravenous benzodiazepines, such as lorazepam or diazepam, as first-line anticonvulsants to terminate the seizures within 5 minutes of administration
- Refractory therapy involves administering intravenous non-benzodiazepine anticonvulsants, such as phenytoin, fosphenytoin, valproate, levetiracetam, or lacosamide, as second-line anticonvulsants to prevent seizure recurrence within 60 minutes of administration
- If seizures persist despite initial and refractory therapy, the patient is considered to have super-refractory SE and may require more aggressive treatment options, such as continuous infusion of anesthetic agents (e.g. propofol), ketamine, or barbiturates (e.g. pentobarbital), or other interventions such as hypothermia or surgery
- The nursing care and management of patients with SE involves:
- Providing a safe and supportive environment for the patient, such as padding the bed rails, removing any potential hazards, maintaining a patent airway, administering oxygen, and suctioning secretions as needed
- Administering anticonvulsant medications as prescribed and monitoring their effectiveness and adverse effects, such as respiratory depression, hypotension, sedation, or allergic reactions
- Monitoring the patient’s vital signs, neurologic status, seizure activity, and EEG findings, and reporting any changes or abnormalities to the health care provider
- Performing frequent blood tests to assess glucose, electrolytes, calcium, magnesium, liver function, renal function, blood cultures, arterial blood gas, and serum anticonvulsant levels, and correcting any imbalances or abnormalities as ordered
- Providing adequate hydration and nutrition to the patient, either orally or parenterally, and preventing aspiration or dehydration
- Preventing complications such as infection, pressure ulcers, contractures, or venous thromboembolism by implementing appropriate measures such as hygiene, skin care, passive range of motion exercises, and prophylactic anticoagulation
- Educating the patient and family about the causes, signs and symptoms, treatment, and prevention of SE and seizures in general, as well as the importance of adherence to anticonvulsant therapy and regular follow-up visits
- Providing emotional support and reassurance to the patient and family and addressing any concerns or fears they may have
- SE is a life-threatening condition that can cause serious complications and poor outcomes if not treated promptly and effectively
- Some of the possible complications include:
- Permanent brain damage or death due to neuronal injury or death, cerebral edema, increased intracranial pressure, or cerebral ischemia
- Respiratory failure or pulmonary edema due to hypoxia, hypercapnia, or aspiration
- Cardiac arrest or arrhythmias due to autonomic instability, hypotension, or electrolyte imbalance
- Shock or multiorgan failure due to hypoperfusion, acidosis, or rhabdomyolysis
- Infection or sepsis due to impaired immunity, invasive procedures, or catheter-associated complications
- The outcomes of SE depend on various factors such as the type, duration, and severity of seizures, the underlying etiology and comorbidities of the patient, and the timeliness and effectiveness of treatment
- Some of the possible outcomes include:
- Complete recovery without any residual neurologic deficits or recurrence of seizures
- Partial recovery with some degree of neurologic impairment or increased frequency or severity of seizures
- Persistent vegetative state or coma due to extensive brain damage or anoxic injury
- Death due to refractory seizures or complications
Epileptic seizures
Causes of epilepsy and seizure disorders
Risk factors of epilepsy and seizure disorders
Signs and symptoms of epilepsy and seizure disorders
Diagnosis of epilepsy and seizure disorders
Treatment of epilepsy and seizure disorders
Treatment of epilepsy and seizure disorders
Status epilepticus.
Causes and risk factors of Status epilepticus.
Pathophysiology of Status epilepticus.
Clinical manifestation of Status epilepticus.
Diagnosis of Status epilepticus.
Treatment of Status epilepticus.
Nursing care and management of Status epilepticus.
Complications and outcomes of Status epilepticus.
Nursing Test Bank
Quiz #1: RN Exams Pharmacology Exams
Quiz #2: RN Exams Medical-Surgical Exams
Quiz #3: RN Exams Fundamentals Exams
Quiz #4: RN Exams Maternal-Newborn Exams
Quiz #5: RN Exams Anatomy and Physiology Exams
Quiz #6: RN Exams Obstetrics and Pediatrics Exams
Quiz #7: RN Exams Fluid and Electrolytes Exams
Quiz #8: RN Exams Community Health Exams
Quiz #9: RN Exams Promoting Health across the lifespan Exams
Quiz #10: RN Exams Multidimensional care Exams
Naxlex Comprehensive Predictor Exams
Quiz #1: Naxlex RN Comprehensive online practice 2019 B with NGN
Quiz #2: Naxlex RN Comprehensive Predictor 2023
Quiz #3: Naxlex RN Comprehensive Predictor 2023 Exit Exam A
Quiz #4: Naxlex HESI Exit LPN Exam
Quiz #5: Naxlex PN Comprehensive Predictor PN 2020
Quiz #6: Naxlex VATI PN Comprehensive Predictor 2020
Quiz #8: Naxlex PN Comprehensive Predictor 2023 - Exam 1
Quiz #10: Naxlex HESI PN Exit exam
Quiz #11: Naxlex HESI PN EXIT Exam 2
Questions on Epilepsy and Seizure Disorders: Status epilepticus
Correct Answer is B
Explanation
This is an incorrect answer. Documenting the onset, duration, and characteristics of the seizure is an important action for the nurse to take for a client who has epilepsy and is experiencing status epilepticus, but it is not the first action. Documentation can provide valuable information for diagnosis, treatment, and evaluation of seizure activity and its effects on the client's condition and quality of life. The nurse should document these details accurately and objectively as soon as possible after the seizure ends. However, before documenting any details, the nurse should ensure that the client's airway and head are protected from injury or obstruction.
Correct Answer is ["A","B","C","E"]
Explanation
This is a correct answer. The nurse should advise the client and their caregiver to perform relaxation techniques such as deep breathing or meditation, as this can help prevent seizures by reducing stress, anxiety, or tension that may trigger seizure activity. Relaxation techniques can also improve mood, sleep quality, and coping skills for the client and their caregiver.
This is a correct answer. The nurse should tell the client that phenytoin can cause gingival hyperplasia, nystagmus, ataxia, or dysrhythmias. These are the common or serious side effects of phenytoin that can affect the oral health, vision, balance, or cardiac function of the client. The nurse shoul
This is an incorrect answer. The nurse should not monitor for hyperglycemia during plasmapheresis for a client who has GBS. Hyperglycemia is not a common complication of plasmapheresis, but rather insulin therapy or steroid therapy, which can increase blood glucose levels in clients who have diabete
Search Here
Related Topics
More on Nursing
- Pathophysiology of the Musculoskeletal System
- Pathophysiology of the Reproductive System
- Pathophysiology of the integumentary system
- Pathophysiology of the Hematologic System
- Pathophysiology of the respiratory system
- Pathophysiology of the renal system
- Pathophysiology of the Gastrointestinal System
- Basic Concepts of Pathophysiology
Free Nursing Study Materials
Access to all study guides and practice questions for nursing for free.
- Free Nursing Study Trials
- Free Nursing Video tutorials
- Free Nursing Practice Tests
- Free Exam and Study Modes
- Free Nursing Revision Quizlets
