Traumatic Brain Injury: Concussions
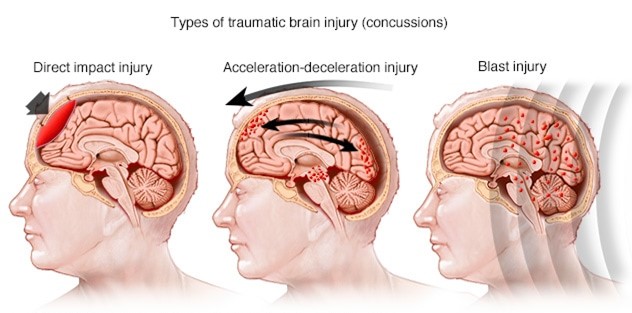
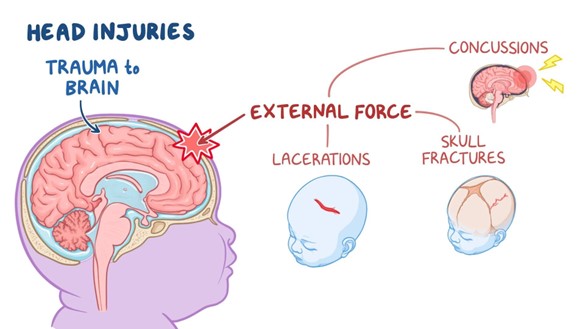
- Traumatic brain injury (TBI) is defined as an alteration in brain function or other evidence of brain pathology caused by an external force3. TBI can result from a direct impact to the head (such as a fall, assault, motor vehicle accident, sports injury, etc.), a penetrating injury (such as a gunshot wound or stab wound), or an indirect injury (such as a blast wave or acceleration-deceleration force)3.
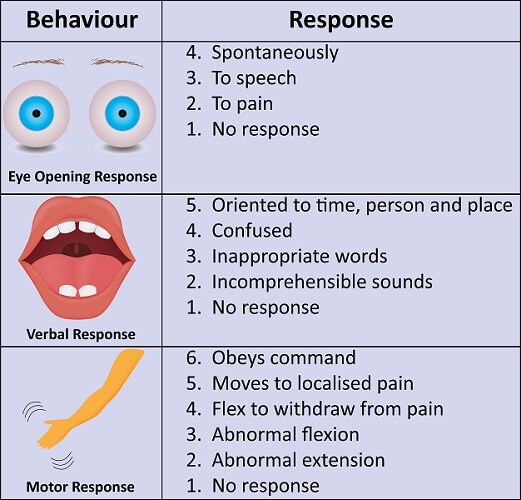
- TBI can be classified according to its severity into mild, moderate, or severe based on the Glasgow Coma Scale (GCS), which measures the level of consciousness by assessing eye opening, verbal response, and motor response4. The GCS ranges from 3 to 15, with lower scores indicating worse outcomes. A mild TBI has a GCS score of 13 to 15; a moderate TBI has a GCS score of 9 to 12; a severe TBI has a GCS score of 8 or less4.
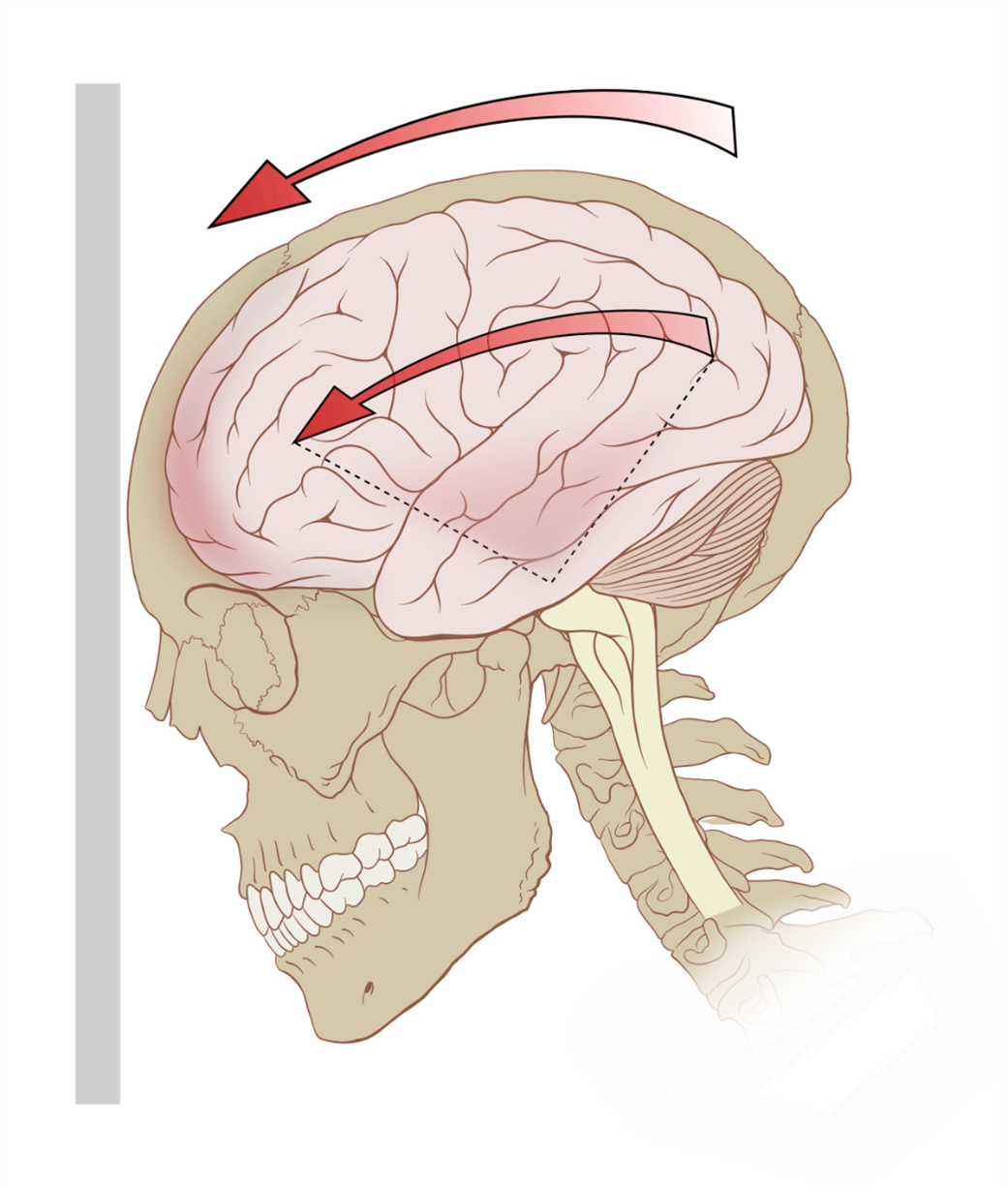
- A concussion is a type of mild TBI that occurs when the brain is rapidly shaken or twisted within the skull due to an external force. This causes stretching or tearing of axons (the long extensions of neurons that transmit signals), disruption of synaptic transmission (the communication between neurons), release of inflammatory mediators (substances that trigger inflammation), alteration of blood flow (the delivery of oxygen and nutrients to the brain), and activation of cell death pathways (the mechanisms that lead to cell death)5.
- A concussion can cause various signs and symptoms that may appear immediately or later after the injury. These include headache, dizziness, nausea, vomiting, fatigue, blurred vision, ringing in the ears, confusion, amnesia (loss of memory), disorientation (loss of sense of direction), difficulty concentrating or remembering information, slurred speech, delayed reaction time, irritability, mood changes, anxiety, depression, insomnia, sensitivity to light or noise, and balance problems5.
- Most concussions resolve within days to weeks with rest and gradual return to normal activities. However, some concussions may have persistent or delayed symptoms that last for months or years. This is known as post-concussion syndrome (PCS)6. PCS can affect physical, cognitive, emotional, and behavioral functioning, and impair quality of life6.
- Some concussions may also increase the risk of developing chronic traumatic encephalopathy (CTE), a progressive neurodegenerative disease that affects people who have had repeated head trauma over time. CTE is characterized by accumulation of abnormal tau protein in the brain, which leads to neuronal loss, brain atrophy, and cognitive impairment7. CTE can cause symptoms such as memory loss, confusion, dementia, personality changes, aggression, depression, suicidal ideation, and parkinsonism.
- The risk factors for TBI and concussion include age, gender, occupation, lifestyle, and medical history.
- TBI and concussion are more common in young children, adolescents, young adults, and older adults, due to their increased exposure to falls, sports injuries, motor vehicle accidents, and violence8.
- Males are more likely than females to sustain TBI and concussion, due to their higher involvement in risky behaviors, physical activities, and occupations8.
- People who work in construction, mining, transportation, military, or law enforcement are also at higher risk of TBI and concussion, due to their exposure to hazards and trauma8.
- People who have a history of substance abuse, mental illness, epilepsy, or previous TBI or concussion are also more prone to TBI and concussion, due to their impaired judgment, coordination, or brain function8.
- The prevention of TBI and concussion involves reducing the exposure to potential causes and increasing the protection of the head.
- Some of the prevention strategies include wearing helmets or seat belts when engaging in activities such as cycling, skiing, riding motorcycles, or driving cars;
- avoiding alcohol or drugs that can impair cognition or motor skills; following safety rules and regulations in sports or workplaces;
- avoiding fights or violence; and seeking medical attention for any neurological symptoms or conditions9.
- The role of nurses in TBI and concussion is to provide screening, assessment, management, education, and support for patients and their families. Nurses can screen patients for TBI and concussion by asking about their history of head trauma, symptoms, and risk factors; performing a physical examination; and using tools such as the GCS or the Sport Concussion Assessment Tool (SCAT)10. Nurses can assess patients for TBI and concussion by monitoring their vital signs (such as blood pressure, pulse, respiration, temperature), neurological status (such as level of consciousness, pupil size and reaction, cranial nerve function), cognitive function (such as orientation, memory, attention, language), emotional state (such as mood, affect, behavior), and functional ability (such as mobility, balance, coordination)10.
- Nurses can manage patients with TBI and concussion by providing interventions such as administering medications (such as analgesics for pain relief, antiemetics for nausea control, anticonvulsants for seizure prevention), maintaining airway patency (such as suctioning secretions, positioning the head midline), ensuring adequate oxygenation (such as administering supplemental oxygen, monitoring oxygen saturation), preventing increased intracranial pressure (ICP) (such as elevating the head of the bed 30 degrees, avoiding coughing or straining), preventing infection (such as using sterile technique for wound care, administering antibiotics), promoting rest and recovery (such as limiting noise and stimulation, encouraging sleep hygiene), and facilitating rehabilitation (such as providing physical, occupational, or speech therapy)10.
- Nurses can educate patients and their families about TBI and concussion by providing information about the causes, mechanisms, signs, symptoms, complications, and outcomes of TBI and concussion; the diagnostic tests and imaging techniques used to evaluate TBI and concussion; the pharmacological and non-pharmacological interventions for TBI and concussion; the prevention strategies for TBI and concussion; the expected course of recovery from TBI and concussion; the possible long-term effects of TBI and concussion; and the available resources and support services for TBI and concussion10.
- Nurses can support patients and their families by providing emotional support (such as listening to their concerns, validating their feelings, offering reassurance), psychosocial support (such as facilitating coping skills, referring to counseling or support groups), and practical support (such as assisting with discharge planning, coordinating care transitions)10.
- The pathophysiological changes that occur in the brain after TBI and concussion involve primary injury and secondary injury.
- Primary injury refers to the immediate damage caused by the external force that disrupts the integrity of the brain tissue.
- Secondary injury refers to the delayed damage caused by the cascade of molecular and cellular events that are triggered by the primary injury11.
- Primary injury can cause various types of brain lesions depending on the nature and magnitude of the external force.
- These include contusions (bruises on the brain surface), lacerations (tears in the brain tissue), hematomas (blood clots within or around the brain), diffuse axonal injury (widespread damage to axons), and penetrating injury (entry of foreign objects into the brain)11.
- Secondary injury can cause various types of brain dysfunction depending on the extent and duration of the molecular and cellular events.
- Molecular and cellular events that contribute to secondary injury are:
- Ischemia (reduced blood flow to the brain), which leads to hypoxia (low oxygen level in the brain), and energy failure (depletion of ATP, the main energy source for cells).
- Excitotoxicity (excessive stimulation of neurons by glutamate, the main excitatory neurotransmitter in the brain), which leads to calcium overload (increased intracellular calcium level in neurons), and oxidative stress (production of reactive oxygen species that damage cell components).
- Inflammation (activation of immune cells and release of inflammatory mediators in the brain), which leads to edema (swelling of the brain tissue), and cytokine storm (overproduction of pro-inflammatory cytokines that worsen inflammation).
- Apoptosis (programmed cell death) and necrosis (uncontrolled cell death) of neurons and glia, which leads to neuronal loss, gliosis (scarring of the brain tissue), and atrophy (shrinking of the brain volume).
- These pathophysiological changes can affect the function of various components of the nervous system, such as:
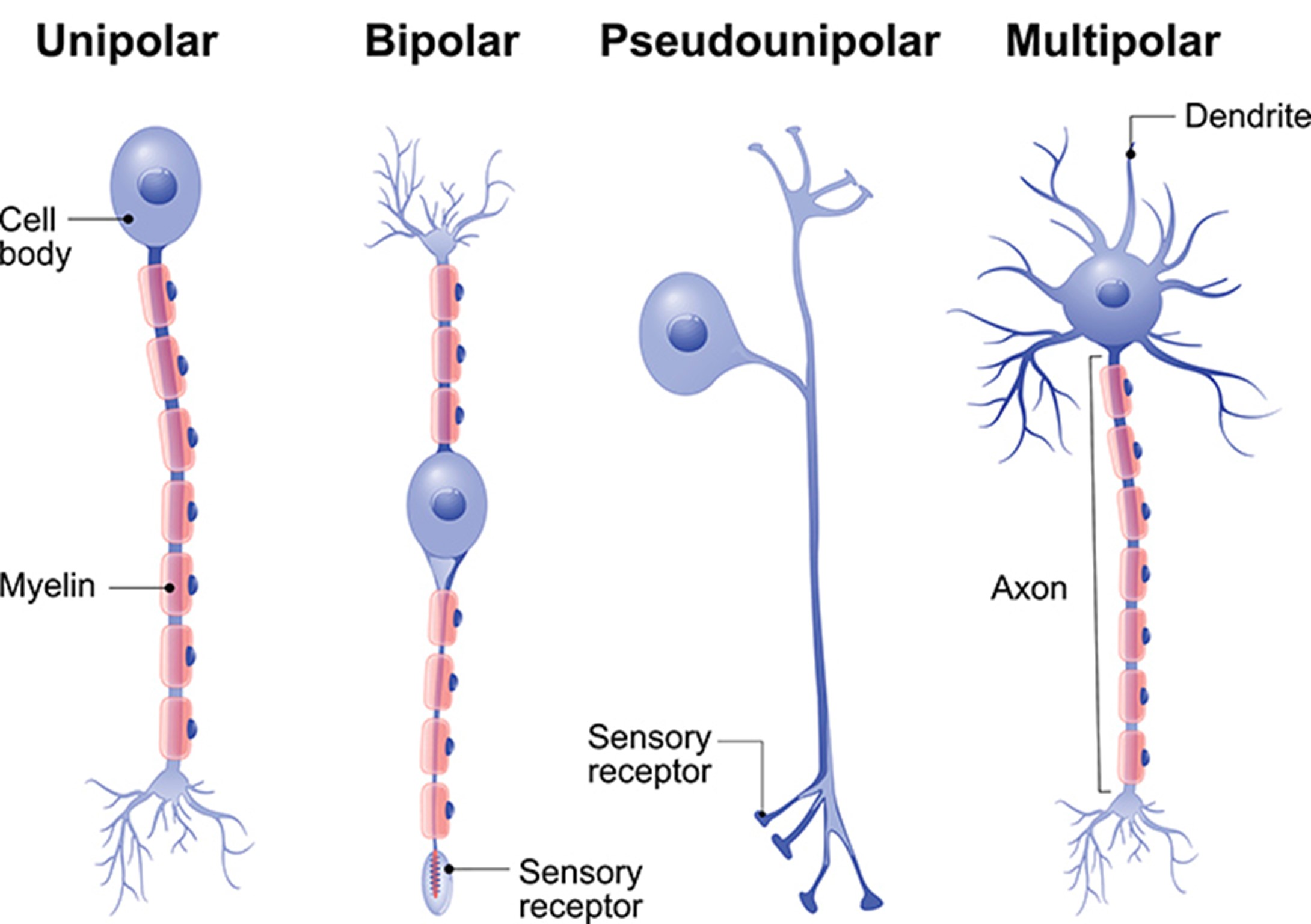
- Neurons, which are the basic units of the nervous system that generate and transmit electrical signals. TBI and concussion can impair the structure and function of neurons by damaging their axons, dendrites, soma, or synapses; altering their membrane potential, action potential, or resting potential; disrupting their neurotransmitter synthesis, release, reuptake, or degradation; and affecting their gene expression, protein synthesis, or metabolism.
- Glia, which are the supporting cells of the nervous system that provide various functions such as insulation, nutrition, protection, and modulation for neurons. TBI and concussion can impair the structure and function of glia by damaging their processes, membranes, or nuclei; altering their proliferation, differentiation, or activation; disrupting their communication with neurons or other glia; and affecting their gene expression, protein synthesis, or metabolism.
- Synapses, which are the junctions between neurons where neurotransmitters are released and received. TBI and concussion can impair the structure and function of synapses by damaging their pre-synaptic terminals, post-synaptic receptors, or synaptic clefts; altering their synaptic strength, plasticity, or pruning; disrupting their neurotransmitter availability, affinity, or efficacy; and affecting their gene expression, protein synthesis, or metabolism.
- Neurotransmitters, which are the chemical messengers that mediate communication between neurons. TBI and concussion can impair the function of neurotransmitters by altering their synthesis, release, reuptake, degradation, or receptor binding; disrupting their balance between excitatory and inhibitory neurotransmitters; and affecting their modulation by other neurotransmitters or neuromodulators.
- Brain regions, which are the specialized areas of the brain that perform specific functions such as sensory processing, motor control, cognitive processing, emotional regulation, memory formation, learning consolidation, behavioral adaptation, autonomic regulation, endocrine regulation, and immune regulation. TBI and concussion can impair the function of brain regions by damaging their anatomical connections, functional networks, or hemispheric dominance; altering their activation, inhibition, or integration; disrupting their coordination, synchronization, or modulation; and affecting their plasticity, adaptability, or resilience.
- The diagnostic tests and imaging techniques used to evaluate TBI and concussion include:
- Neurological examination: A clinical assessment of the patient’s level of consciousness, mental status, cranial nerve function, motor function, sensory function, reflexes, coordination, and balance. This can help determine the severity and location of brain injury and monitor any changes over time.
- Glasgow Coma Scale (GCS): A numerical scale that measures the level of consciousness by assessing eye opening, verbal response, and motor response. This can help classify TBI into mild, moderate, or severe and predict outcomes.
- Sport Concussion Assessment Tool (SCAT): A standardized tool that assesses concussion symptoms, cognitive function, balance performance, and neck examination. This can help diagnose concussion and guide return-to-play decisions.
- Neuropsychological tests: A series of tests that measure cognitive functions such as attention, memory, language, executive function, visuospatial function, and processing speed. This can help identify cognitive impairments and monitor recovery.
- Blood tests: A collection of blood samples that measure biomarkers such as proteins or enzymes that are released from damaged brain cells. This can help detect brain injury and estimate its severity.
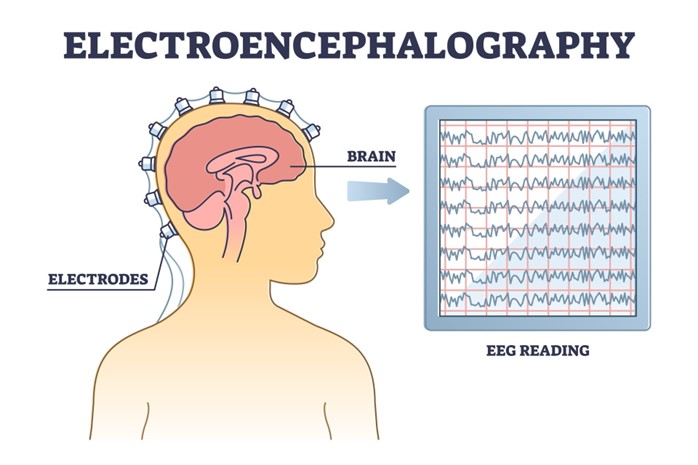
- Electroencephalogram (EEG): A recording of electrical activity in the brain using electrodes attached to the scalp. This can help detect abnormal brain waves or seizures that may occur after TBI or concussion.
- Evoked potentials (EPs): A recording of electrical responses in the brain to specific stimuli such as sounds or flashes. This can help assess the integrity of sensory pathways or cortical function that may be affected by TBI or concussion.
- Computed tomography (CT) scan: An imaging technique that uses x-rays to produce cross-sectional images of the brain. This can help visualize brain structures and detect brain lesions such as contusions, hematomas, or fractures that may occur after TBI or concussion.
- Magnetic resonance imaging (MRI) scan: An imaging technique that uses magnetic fields and radio waves to produce detailed images of the brain. This can help visualize brain structures and detect brain lesions such as diffuse axonal injury, edema, or atrophy that may occur after TBI or concussion.
- Diffusion tensor imaging (DTI) scan: A type of MRI scan that measures the diffusion of water molecules in the brain. This can help visualize brain connections and detect axonal damage that may occur after TBI or concussion.
- Functional MRI (fMRI) scan: A type of MRI scan that measures blood flow in the brain. This can help visualize brain activity and detect functional changes that may occur after TBI or concussion.
- Positron emission tomography (PET) scan: An imaging technique that uses radioactive tracers to measure metabolic activity in the brain. This can help visualize brain activity and detect metabolic changes that may occur after TBI or concussion.
- Neurological examination: It is simple, quick, and inexpensive, but it is subjective, variable, and insensitive to subtle changes.
- Glasgow Coma Scale (GCS): It is simple, quick, and widely used, but it is subjective, variable, and insensitive to mild TBI or concussion.
- Sport Concussion Assessment Tool (SCAT): It is standardized, comprehensive, and sensitive to concussion, but it is time-consuming, variable, and dependent on baseline data.
- Neuropsychological tests: They are objective, reliable, and sensitive to cognitive impairments, but they are time-consuming, expensive, and dependent on baseline data.
- Blood tests: They are objective, reliable, and sensitive to brain injury, but they are invasive, expensive, and dependent on timing and cutoff values.
- Electroencephalogram (EEG): It is non-invasive, inexpensive, and sensitive to abnormal brain activity or seizures, but it is noisy, variable, and dependent on expertise and interpretation.
- Evoked potentials (EPs): They are non-invasive, inexpensive, and sensitive to sensory or cortical dysfunction, but they are noisy, variable, and dependent on expertise and interpretation.
- Computed tomography (CT) scan: It is fast, widely available, and sensitive to structural lesions such as contusions, hematomas, or fractures, but it is invasive, expensive, and exposes the patient to radiation.
- Magnetic resonance imaging (MRI) scan: It is non-invasive, high-resolution, and sensitive to structural lesions such as diffuse axonal injury, edema, or atrophy, but it is slow, expensive, and contraindicated for patients with metal implants or claustrophobia.
- Diffusion tensor imaging (DTI) scan: It is non-invasive, high-resolution, and sensitive to axonal damage, but it is slow, expensive, and dependent on expertise and interpretation.
- Functional MRI (fMRI) scan: It is non-invasive, high-resolution, and sensitive to functional changes, but it is slow, expensive, and dependent on task design and performance.
- Positron emission tomography (PET) scan: It is non-invasive, high-resolution, and sensitive to metabolic changes, but it is slow, expensive, and exposes the patient to radiation.
- Pharmacological interventions: These are medications that are used to treat or prevent various symptoms or complications of TBI and concussion, such as pain, nausea, vomiting, seizures, intracranial hypertension, cerebral edema, infection, inflammation, depression, anxiety, insomnia, or cognitive impairment. Some of the pharmacological interventions for TBI and concussion are:
- Analgesics: These are medications that relieve pain by blocking pain signals or reducing inflammation. Examples of analgesics include acetaminophen, ibuprofen, naproxen, aspirin, tramadol, morphine, fentanyl, and ketamine.
- Antiemetics: These are medications that prevent or reduce nausea and vomiting by blocking receptors in the brain or gastrointestinal tract that trigger these symptoms. Examples of antiemetics include ondansetron, metoclopramide, promethazine, and scopolamine.
- Anticonvulsants: These are medications that prevent or stop seizures by stabilizing the electrical activity of neurons or enhancing the inhibitory effects of gamma-aminobutyric acid (GABA), the main inhibitory neurotransmitter in the brain. Examples of anticonvulsants include phenytoin, carbamazepine, valproic acid, levetiracetam, and lorazepam.
- Osmotic agents: These are medications that reduce intracranial pressure (ICP) and cerebral edema by drawing water out of the brain tissue into the blood vessels. Examples of osmotic agents include mannitol and hypertonic saline.
- Antibiotics: These are medications that prevent or treat infection by killing or inhibiting the growth of bacteria. Examples of antibiotics include ceftriaxone, vancomycin, metronidazole, and meropenem.
- Corticosteroids: These are medications that reduce inflammation by suppressing the immune system and inhibiting the production of inflammatory mediators. Examples of corticosteroids include dexamethasone and methylprednisolone.
- Antidepressants: These are medications that treat depression by increasing the availability or efficacy of serotonin, norepinephrine, or dopamine, the main mood-regulating neurotransmitters in the brain. Examples of antidepressants include selective serotonin reuptake inhibitors (SSRIs) such as fluoxetine, sertraline, and citalopram; serotonin-norepinephrine reuptake inhibitors (SNRIs) such as venlafaxine, duloxetine, and desvenlafaxine; and dopamine-norepinephrine reuptake inhibitors (DNRIs) such as bupropion.
- Anxiolytics: These are medications that treat anxiety by enhancing the inhibitory effects of GABA or reducing the activity of noradrenaline, a neurotransmitter that mediates stress responses. Examples of anxiolytics include benzodiazepines such as diazepam, alprazolam, and clonazepam; and beta-blockers such as propranolol, atenolol, and metoprolol.
- Hypnotics: These are medications that induce or maintain sleep by enhancing the inhibitory effects of GABA or melatonin, a hormone that regulates circadian rhythms. Examples of hypnotics include zolpidem, zaleplon, eszopiclone, and melatonin.
- Cognitive enhancers: These are medications that improve cognitive function by modulating the activity of acetylcholine, glutamate, or dopamine, neurotransmitters that are involved in learning, memory, attention, and executive function. Examples of cognitive enhancers include cholinesterase inhibitors such as donepezil, rivastigmine, and galantamine; N-methyl-D-aspartate (NMDA) receptor antagonists such as memantine; and dopamine agonists such as methylphenidate and modafinil.
- The indications, contraindications, side effects, and nursing implications of these pharmacological interventions depend on various factors such as the type, severity, and duration of TBI or concussion; the patient’s age, weight, medical history, allergies, and current medications; the drug’s dose, route, frequency, and duration; and the drug’s pharmacokinetics (how it is absorbed, distributed, metabolized, and excreted) and pharmacodynamics (how it interacts with its target receptors).
- Therefore, nurses should consult with physicians or pharmacists before administering any medication to patients with TBI or concussion; monitor patients for any adverse reactions or interactions; educate patients about the purpose, benefits, risks, and precautions of the medication; and document the medication administration and patient response.
- Non-pharmacological interventions: These are interventions that do not involve medications but use other methods such as physical, occupational, or speech therapy; cognitive behavioral therapy (CBT); biofeedback; neurofeedback; transcranial magnetic stimulation (TMS); transcranial direct current stimulation (tDCS); or acupuncture to treat or prevent various symptoms or complications of TBI or concussion, such as pain, nausea, vomiting, seizures, intracranial hypertension, cerebral edema, infection, inflammation, depression, anxiety, insomnia, or cognitive impairment. Some of the non-pharmacological interventions for TBI and concussion are:
- Physical therapy: This is a type of therapy that uses exercises, stretches, massages, heat, cold, electrical stimulation, or ultrasound to improve the patient’s physical function, mobility, strength, endurance, balance, and coordination. Physical therapy can help patients with TBI or concussion recover from motor impairments, spasticity, contractures, pain, or fatigue.
- Occupational therapy: This is a type of therapy that uses activities of daily living (ADLs), instrumental activities of daily living (IADLs), leisure activities, or work-related tasks to improve the patient’s functional ability, independence, self-care, and quality of life. Occupational therapy can help patients with TBI or concussion recover from sensory impairments, visual impairments, perceptual impairments, cognitive impairments, or behavioral impairments.
- Speech therapy: This is a type of therapy that uses exercises, games, drills, strategies, or devices to improve the patient’s speech, language, communication, swallowing, or cognition. Speech therapy can help patients with TBI or concussion recover from aphasia (language impairment), dysarthria (speech impairment), apraxia (motor speech impairment), dysphagia (swallowing impairment), or cognitive-communication impairment.
- Cognitive behavioral therapy (CBT): This is a type of psychotherapy that uses cognitive techniques (such as identifying and challenging negative thoughts), behavioral techniques (such as exposure and response prevention), and emotional techniques (such as relaxation and mindfulness) to help the patient cope with psychological symptoms such as depression, anxiety, insomnia, or post-traumatic stress disorder (PTSD). CBT can help patients with TBI or concussion modify their maladaptive beliefs, behaviors, and emotions that result from their brain injury.
- Biofeedback: This is a type of therapy that uses sensors and monitors to measure the patient’s physiological responses such as heart rate, blood pressure, muscle tension, skin temperature, or brain waves. The patient then receives feedback on these responses through visual, auditory, or tactile cues, and learns to control them through relaxation or cognitive techniques. Biofeedback can help patients with TBI or concussion reduce stress, pain, anxiety, or insomnia, and improve autonomic regulation, mood, or cognition.
-
- Neurofeedback: This is a type of biofeedback that uses electroencephalogram (EEG) to measure the patient’s brain waves and provide feedback on their frequency, amplitude, or coherence. The patient then learns to modify their brain waves through operant conditioning or neurostimulation techniques. Neurofeedback can help patients with TBI or concussion enhance brain function, neuroplasticity, or recovery by increasing or decreasing specific brain wave patterns that are associated with different cognitive or emotional states.
- Transcranial magnetic stimulation (TMS): This is a type of therapy that uses a coil to generate a magnetic field that induces an electric current in the brain. The current then stimulates or inhibits specific brain regions or networks that are involved in various functions such as motor control, language, memory, attention, emotion, or mood. TMS can help patients with TBI or concussion improve neurological function, cognitive function, or psychiatric symptoms by modulating the activity of the targeted brain regions or networks.
- Transcranial direct current stimulation (tDCS): This is a type of therapy that uses electrodes to deliver a low-intensity direct current to the scalp. The current then alters the excitability of the underlying brain tissue by depolarizing or hyperpolarizing the neurons. tDCS can help patients with TBI or concussion improve neurological function, cognitive function, or psychiatric symptoms by enhancing or suppressing the activity of the affected brain regions.
- Acupuncture: This is a type of therapy that uses needles to stimulate specific points on the body that are connected to different organs or systems. Acupuncture can help patients with TBI or concussion reduce pain, inflammation, nausea, vomiting, anxiety, depression, insomnia, or cognitive impairment by regulating the flow of qi (vital energy) and blood in the body.
- The indications, contraindications, side effects, and nursing implications of these non-pharmacological interventions depend on various factors such as the type, severity, and duration of TBI or concussion; the patient’s age, weight, medical history, allergies, and current medications; the intervention’s dose, frequency, and duration; and the intervention’s mechanism of action and evidence base. Therefore, nurses should consult with physicians or therapists before recommending or administering any non-pharmacological intervention to patients with TBI or concussion; monitor patients for any adverse reactions or interactions; educate patients about the purpose, benefits, risks, and precautions of the intervention; and document the intervention administration and patient response.
Risk Factors and Prevention of concussion
Role of Nurses
Pathophysiological Changes
Diagnostic Tests and Imaging Techniques
The advantages and limitations of these diagnostic tests and imaging techniques are:
Pharmacological and Non-pharmacological Interventions
The pharmacological and non-pharmacological interventions for TBI and concussion include:
Nursing Test Bank
Quiz #1: RN Exams Pharmacology Exams
Quiz #2: RN Exams Medical-Surgical Exams
Quiz #3: RN Exams Fundamentals Exams
Quiz #4: RN Exams Maternal-Newborn Exams
Quiz #5: RN Exams Anatomy and Physiology Exams
Quiz #6: RN Exams Obstetrics and Pediatrics Exams
Quiz #7: RN Exams Fluid and Electrolytes Exams
Quiz #8: RN Exams Community Health Exams
Quiz #9: RN Exams Promoting Health across the lifespan Exams
Quiz #10: RN Exams Multidimensional care Exams
Naxlex Comprehensive Predictor Exams
Quiz #1: Naxlex RN Comprehensive online practice 2019 B with NGN
Quiz #2: Naxlex RN Comprehensive Predictor 2023
Quiz #3: Naxlex RN Comprehensive Predictor 2023 Exit Exam A
Quiz #4: Naxlex HESI Exit LPN Exam
Quiz #5: Naxlex PN Comprehensive Predictor PN 2020
Quiz #6: Naxlex VATI PN Comprehensive Predictor 2020
Quiz #8: Naxlex PN Comprehensive Predictor 2023 - Exam 1
Quiz #10: Naxlex HESI PN Exit exam
Quiz #11: Naxlex HESI PN EXIT Exam 2
Questions on Traumatic Brain Injury: Concussions
Correct Answer is D
Explanation
This is a correct answer. All of the above are possible symptoms of CTE, which can vary in severity and onset depending on the individual and the extent of brain damage. Other possible symptoms include confusion, cognitive impairment, speech problems, vision problems, balance problems, motor problems, or suicidal thoughts.
Correct Answer is ["A","B","C","E"]
Explanation
This is a correct answer. Educating the client about the signs of post-concussion syndrome helps to prepare them for possible complications and when to seek medical attention. Post-concussion syndrome is a condition in which symptoms persist for weeks or months after a concussion. Symptoms may include headache, dizziness, fatigue, insomnia, anxiety, depression, or cognitive impairment.
Correct Answer is C
Explanation
This is an incorrect answer. The nurse should not advise the client to ask their coach or trainer what they think. The coach or trainer may not be qualified or knowledgeable enough to assess the client's condition and readiness to return to sports or other physical activities. The client should rely on their doctor's advice and not on their coach's or trainer's opinion.
Correct Answer is C
Explanation
This is an incorrect answer. The client does not need further teaching if they say they will have someone stay with them for the next 24 hours. Having someone stay with them is a recommended precaution after a concussion. The person can observe the client for any signs of worsening brain injury such as confusion, vomiting, seizures, or loss of consciousness and call for help if needed.
This is an incorrect answer. The nurse should not instruct the client to take ibuprofen or aspirin for pain relief after a concussion. Ibuprofen and aspirin are nonsteroidal anti-inflammatory drugs (NSAIDs) that can increase the risk of bleeding in the brain or interfere with blood clotting.
This is an incorrect answer. Notifying the provider of the client's condition is an important action for the nurse to take, but not the first one. The nurse should first assess the client's neurological status and gather relevant data before reporting to the provider.
This is an incorrect answer. The client does not need immediate reporting if they have difficulty performing finger-to-nose test. This is an abnormal finding that indicates cerebellar dysfunction, which affects coordination and balance. However, it does not indicate an acute or urgent condition, but
This is a correct answer. Drinking plenty of fluids and eating a balanced diet after a concussion helps to promote healing and recovery by providing hydration and nutrition to the brain and body.
Search Here
Related Topics
More on Nursing
- Pathophysiology of the Musculoskeletal System
- Pathophysiology of the Reproductive System
- Pathophysiology of the integumentary system
- Pathophysiology of the Hematologic System
- Pathophysiology of the respiratory system
- Pathophysiology of the renal system
- Pathophysiology of the Gastrointestinal System
- Basic Concepts of Pathophysiology
Free Nursing Study Materials
Access to all study guides and practice questions for nursing for free.
- Free Nursing Study Trials
- Free Nursing Video tutorials
- Free Nursing Practice Tests
- Free Exam and Study Modes
- Free Nursing Revision Quizlets
