A client is prescribed alprazolam for acute anxiety. What client history should cause a nurse to question this order?
A personality disorder.
Hypertension.
Alcohol use disorder.
Schizophrenia.
The Correct Answer is C
Choice A Reason
While a personality disorder can present challenges in managing medications due to the complexity of the psychiatric condition, it is not typically a contraindication for the use of alprazolam. However, caution is advised as the dynamics of personality disorders can affect medication adherence and response.
Choice B Reason
Hypertension is not a direct contraindication for alprazolam. However, since alprazolam can sometimes cause changes in blood pressure, it is important for the nurse to monitor the client's blood pressure and consult with the physician if there are concerns.
Choice C Reason
Alcohol use disorder is a significant concern when prescribing alprazolam. Alprazolam is a benzodiazepine, and concurrent use with substances like alcohol can increase the risk of respiratory depression, sedation, and misuse or addiction. Therefore, a history of alcohol use disorder should prompt the nurse to question the order and discuss alternative treatments with the physician.
Choice D Reason
Schizophrenia itself is not a contraindication for the use of alprazolam, but it is essential to consider the overall treatment plan for the client. Alprazolam is not a primary treatment for schizophrenia and is used for anxiety management. The nurse should ensure that the use of alprazolam does not interfere with the treatment of schizophrenia.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
Choice A Reason
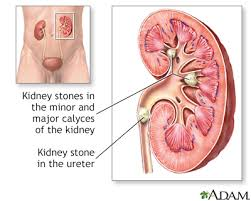
Increasing sodium intake is not recommended for patients who have passed a calcium oxalate stone. High sodium intake can increase calcium in the urine, which can contribute to the formation of new stones. Therefore, patients are often advised to limit their sodium intake to reduce the risk of stone recurrence.
Choice B Reason
Considering a move to an area with higher humidity is not a standard recommendation for preventing the recurrence of calcium oxalate stones. While climate can affect hydration levels, it is more important for the patient to focus on direct measures to stay hydrated, such as drinking more fluids.
Choice C Reason
Increasing water intake is a key recommendation for patients who have had calcium oxalate stones. Adequate hydration is essential to dilute the urine, which helps prevent the formation of new stones. Patients are often advised to drink enough water to produce at least 2.5 liters of urine per day.
Choice D Reason
Decreasing the intake of all calcium-rich foods and beverages is not generally recommended for patients with calcium oxalate stones. In fact, a moderate intake of dietary calcium can help reduce the risk of stone formation by binding with oxalate in the intestines, which prevents it from being absorbed into the urine. Patients should consult with a healthcare provider or dietitian to determine the appropriate amount of dietary calcium.
Correct Answer is C
Explanation
Choice a reason:
Placing the client on 2L via nasal cannula is a common intervention for hypoxemia, but with the client's pulse oximetry at 88%, which is below the normal range of 95-100%, and the presence of tachypnea, a more immediate assessment of the client's respiratory status is warranted. Oxygen therapy should be guided by the results of arterial blood gas (ABG) analysis to tailor the treatment to the client's specific needs.
Choice b reason:
Obtaining a blood glucose level is not the most immediate concern in the context of altered mental status and respiratory distress. While it is important to rule out hypoglycemia as a cause of altered mental status, the primary concern indicated by the vital signs is the client's respiratory condition.
Choice c reason:
Calling the physician for an order for a stat arterial blood gas is the most appropriate action. The ABG will provide detailed information about the client's oxygenation, carbon dioxide levels, and acid-base balance. This is crucial for a client with a new onset change in mental status and tachypnea, as it can indicate respiratory failure or other serious complications of pneumonia.
Choice d reason:
Requesting an order for lorazepam is not appropriate given the client's current respiratory status. Lorazepam, a benzodiazepine, can depress the central nervous system and respiratory drive, potentially worsening the client's hypoxemia and respiratory effort.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
