A female college student comes to the school's health clinic complaining of urinary frequency and burning with right lower back pain. Which intervention should the nurse implement first?
Evaluate the urine for a strong odor.
Measure her temperature and pulse rate
Test her urine for the presence of hematuria.
Palpate the right flank for tenderness
The Correct Answer is B
A. Evaluate the urine for a strong odor.
While evaluating urine for a strong odor can provide some information about a possible urinary tract infection (UTI), it is not the most immediate concern. The priority in this case is to assess for signs of systemic infection, and checking for a strong odor can be done later.
B. Measure her temperature and pulse rate.
This is the correct choice. Measuring temperature and pulse rate is a critical initial step to assess for signs of systemic infection. Fever and an elevated pulse rate can indicate that the infection may have spread beyond the bladder, possibly involving the kidneys.
C. Test her urine for the presence of hematuria.
Testing for hematuria (blood in the urine) is an important diagnostic step for a UTI, but it is not the first priority. Vital sign assessment takes precedence to determine the severity of the condition and the need for urgent intervention.
D. Palpate the right flank for tenderness.
Palpating the right flank for tenderness is a relevant physical assessment to check for kidney involvement, which is important in cases of suspected pyelonephritis. However, assessing vital signs is a more immediate and critical step to determine the severity of the condition.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
A. Evaluate upper and lower extremities for perfusion, pulse volume, and pitting edema:
This option focuses on assessing perfusion and circulation in the extremities. While it's important in certain situations, in the context of a client who recently underwent cardiac stent placement and is now experiencing chest pressure and shortness of breath, the priority is to assess the cardiac status more directly.
B. Listen for extra heart sounds, murmurs, and rhythm with the bell of the stethoscope:
This option involves auscultating the heart for abnormal sounds or rhythms. While it's a valuable assessment in general, in this particular scenario, obtaining an electrocardiogram (ECG) and initiating continuous cardiac monitoring would provide a more comprehensive and immediate evaluation of the cardiac status.
C. Obtain a 12-lead electrocardiogram and begin continuous cardiac monitoring:
This is the correct choice. Obtaining a 12-lead ECG and initiating continuous cardiac monitoring is crucial in assessing the client's cardiac function. It allows for the detection of any acute changes in the heart's electrical activity or rhythm, which is essential for timely intervention and management.
D. Verify troponin level assessments are scheduled every 3-6 hours for a series of three:
Monitoring troponin levels is important in assessing cardiac damage, but in this acute situation, obtaining an immediate ECG and initiating continuous cardiac monitoring take precedence for a more real-time evaluation of the client's cardiac status. Troponin levels may be monitored subsequently based on the initial findings.
Correct Answer is D
Explanation
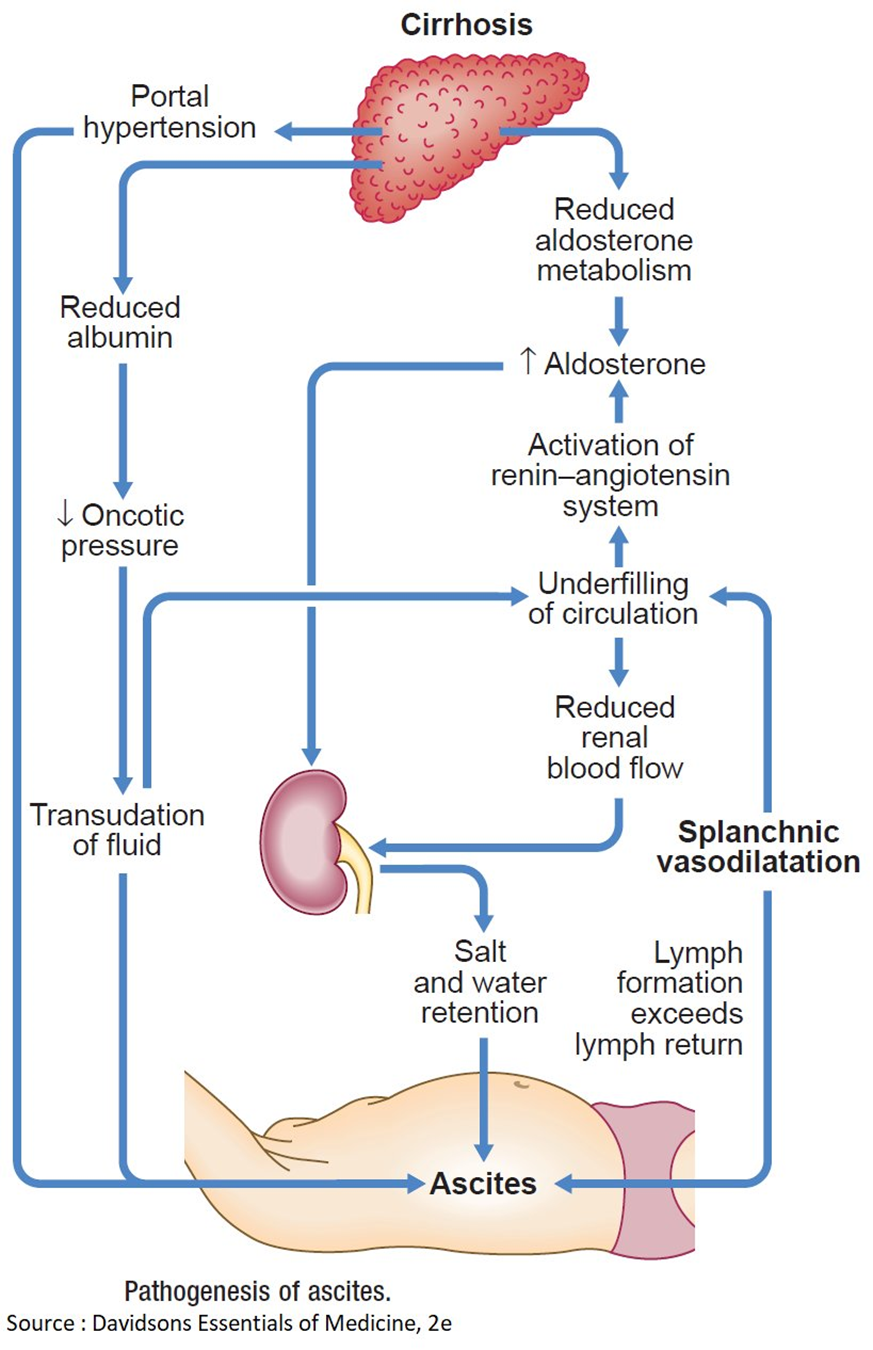
A. Hyperaldosteronism causing an increased sodium reabsorption in renal tubules.
Hyperaldosteronism is characterized by an excess of aldosterone, a hormone that regulates sodium and water balance. In cirrhosis, however, sodium retention is often related to other mechanisms such as portal hypertension and hypoalbuminemia, rather than hyperaldosteronism.
B. Decreased renin-angiotensin response related to an increase in renal blood flow.
Cirrhosis is more commonly associated with an activated renin-angiotensin-aldosterone system, leading to increased sodium and water retention. The increased renin-angiotensin response is a compensatory mechanism to maintain perfusion in the setting of cirrhosis and does not contribute to decreased renal blood flow.
C. Decreased portacaval pressure with greater collateral circulation.
This statement is not accurate. In cirrhosis, there is typically increased portacaval pressure due to portal hypertension, which can lead to the development of collateral circulation. However, this does not explain the edema and ascites seen in cirrhosis.
D. Hypoalbuminemia that results in a decreased colloidal oncotic pressure.
This is the correct choice. In cirrhosis, liver damage leads to decreased synthesis of albumin. Albumin plays a crucial role in maintaining colloidal oncotic pressure, and when it is decreased (hypoalbuminemia), fluid is more likely to leak out of blood vessels, resulting in edema. The same mechanism contributes to the development of ascites in the abdominal cavity.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
