A few days after a Cerebral Vascular Accident, the patient's family asks the nurse if tissue plasminogen activator (tPA) is a drug therapy option now. The nurse's response based on the knowledge that this drug must be used within:
4 hours
1 hour
24 hours
8 hours
The Correct Answer is A
A. 4 hours:
This option indicates that tissue plasminogen activator (tPA) must be administered within 4 hours of the onset of stroke symptoms to be considered as a drug therapy option. tPA is a thrombolytic medication used to dissolve blood clots in ischemic stroke, and its effectiveness is highest when administered promptly after the onset of symptoms.
B. 1 hour:
Administering tPA within 1 hour of stroke onset would be extremely challenging and impractical. It typically takes time for patients to recognize stroke symptoms, seek medical attention, and undergo diagnostic evaluations before tPA administration. While time is of the essence in stroke treatment, 1 hour is too short of a timeframe for most patients to receive tPA.
C. 24 hours:
Administering tPA beyond 4.5 hours of stroke onset is generally contraindicated due to the increased risk of complications, including hemorrhagic transformation of the stroke. While there may be some extended time windows considered for certain patients under specific circumstances, such as those meeting eligibility criteria for extended thrombolytic therapy, 24 hours is outside the standard timeframe for tPA administration.
D. 8 hours:
While tPA administration within 8 hours of stroke onset may be feasible for some patients, it is beyond the standard recommended time window for optimal effectiveness. As mentioned earlier, tPA is most effective when administered within the first 3 to 4.5 hours after the onset of symptoms, with earlier administration associated with better outcomes.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is ["A","B","C","D","E","F"]
Explanation
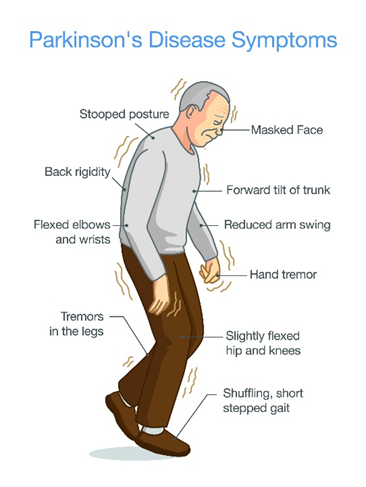
A. Muscle tremors:
Muscle tremors, particularly resting tremors, are a hallmark feature of Parkinson's disease. These tremors typically occur in the hands, fingers, arms, legs, jaw, or head and may worsen with stress or inactivity.
B. Slow body movement (bradykinesia):
Bradykinesia refers to slowness of movement and is another key symptom of Parkinson's disease. Patients may have difficulty initiating movement, experience a decrease in spontaneous movement (hypokinesia), and demonstrate reduced range of motion.
C. Rigidity:
Rigidity, or stiffness of the muscles, is a common symptom of Parkinson's disease. It often affects the limbs and trunk and can contribute to difficulty with movement and posture.
D. Pill rolling:
Pill rolling refers to a specific type of tremor characterized by rhythmic, rolling movements of the thumb and fingers, resembling the action of rolling a pill between the fingers and thumb. This tremor is commonly seen in Parkinson's disease.
E. Lack of facial expression:
Parkinson's disease can lead to a reduced range of facial expressions, also known as hypomimia or "masked facies." Patients may have a fixed, expressionless facial appearance and reduced blinking.
F. Drooling:
Drooling, or excessive salivation, can occur in Parkinson's disease due to impaired swallowing function (dysphagia) and reduced control over oral and facial muscles.
Correct Answer is ["15"]
Explanation
To calculate the dose of amantadine for a client with parkinsonism, the nurse needs to use the following formula:
Dose (mL) = Ordered dose (mg) / Concentration (mg/mL).
In this case, the ordered dose is 150 mg and the concentration is 50 mg/5 mL. Therefore, the dose in mL is:
Dose (mL) = 150 mg / (50 mg/5 mL)
Dose (mL) = 150 mg x (5 mL/50 mg)
Dose (mL) = 15 mL
The nurse should round the answer to the nearest whole number, which is 15 mL. The nurse should administer 15 mL of amantadine oral solution to the client.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
