A newborn has meconium aspiration at birth. The nurse notes increasing respiratory distress. What action takes priority?
Obtain an oxygen saturation.
Stimulate the baby to increase respirations.
Prepare to initiate ECMO.
Notify the provider at once.
The Correct Answer is D
Choice A) Obtain an oxygen saturation: This is not a priority action because it does not address the underlying cause of the respiratory distress, which is meconium aspiration. Meconium aspiration can cause airway obstruction, inflammation, infection, and pulmonary hypertension in the newborn. Oxygen saturation may be low, but it is not a reliable indicator of the severity of the condition.
Choice B) Stimulate the baby to increase respirations: This is not a priority action because it may worsen the respiratory distress by increasing the work of breathing and causing more meconium to be aspirated. Stimulation may also cause stress and hypoxia in the newborn.
Choice C) Prepare to initiate ECMO: This is not a priority action because it is a last resort treatment for severe cases of meconium aspiration syndrome that do not respond to conventional therapies. ECMO stands for extracorporeal membrane oxygenation, which is a form of life support that bypasses the lungs and provides oxygen to the blood.
ECMO has many risks and complications, such as bleeding, infection, and organ damage. It should only be used when other options have failed and with the consent of the parents.
Choice D) Notify the provider at once: This is the correct action because it allows for prompt assessment and intervention by the provider, who can initiate appropriate treatments for meconium aspiration syndrome. These may include suctioning of the airway, administration of antibiotics, surfactant, or inhaled nitric oxide, and mechanical ventilation . Early treatment can improve the outcomes and reduce the complications of meconium aspiration syndrome.

Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
Choice A) Report of absent breast pain is incorrect because this is not a finding that indicates that the medication was effective, but rather a finding that indicates that the client does not have mastitis or engorgement. Mastitis is an infection of the breast tissue that causes pain, swelling, redness, and fever. Engorgement is a condition where the breasts become overfilled with milk, causing pain, hardness, and leakage. Both conditions are common in postpartum women who are breastfeeding, but they are not related to methylergonovine or uterine bleeding. Therefore, this response is irrelevant and inaccurate.
Choice B) Increase in lochia is incorrect because this is not a finding that indicates that the medication was effective, but rather a finding that indicates that the medication was ineffective or that the client has a complication. Lochia is the vaginal discharge that consists of blood, mucus, and tissue from the uterus after childbirth. It usually lasts for about 4 to 6 weeks and gradually decreases in amount and color. Methylergonovine is a medication that helps to control uterine bleeding by improving the tone and contractions of the uterus. An increase in lochia may mean that methylergonovine did not work well or that the client has a problem such as retained placenta, infection, or subinvolution. Therefore, this response is opposite and inaccurate.
Choice C) Increase in blood pressure is incorrect because this is not a finding that indicates that the medication was effective, but rather a finding that indicates that the client has a side effect or a risk factor. Blood pressure is the force of blood against the walls of the arteries. It is measured by two numbers: systolic (the pressure when the heart beats) and diastolic (the pressure when the heart rests). The normal range for blood pressure is 120/80 mm Hg or lower. Methylergonovine is a medication that can cause vasoconstriction, which means narrowing of the blood vessels and increasing of the blood pressure. This can lead to complications such as hypertension, stroke, or heart attack. Therefore, this response is adverse and inaccurate.
Choice D) Fundus firm to palpation is correct because this is a finding that indicates that the medication was effective and that the client has a good outcome. The fundus is the upper part of the uterus that can be felt through the abdomen after childbirth. It should be firm, midline, and at or below the level of the navel. A firm fundus means that the uterus has contracted well and stopped bleeding. Methylergonovine is a medication that helps to achieve this by improving the tone and contractions of the uterus. Therefore, this response is positive and accurate.

Correct Answer is D
Explanation
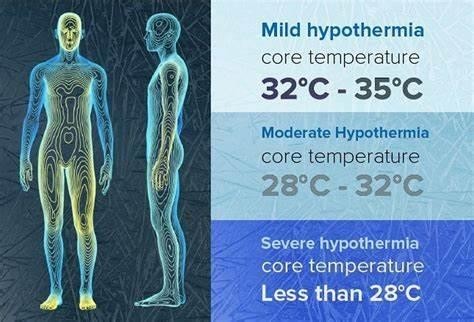
Choice A) Decreased metabolic rate is incorrect because this is not a result of hypothermia in the newborn, but rather a cause of it. Metabolic rate is the speed at which the body uses energy to perform its functions. Newborns have a high metabolic rate, which helps them to maintain a normal body temperature of 36.5°C to 37.5°C (97.7°F to 99.5°F). However, some factors can lower the metabolic rate of newborns, such as prematurity, low birth weight, infection, or hypoglycemia. A low metabolic rate can make the newborn more susceptible to heat loss and hypothermia, which is a condition that occurs when the body temperature drops below 36°C (96.8°F). Therefore, this response is inaccurate and misleading.
Choice B) Decreased oxygen demands is incorrect because this is not a result of hypothermia in the newborn, but rather a consequence of it. Oxygen demand is the amount of oxygen that the body needs to function properly.
Newborns have a high oxygen demand, which helps them to support their growth and development. However, some factors can decrease the oxygen demand of newborns, such as hypothermia, sedation, or asphyxia. A low oxygen demand can impair the oxygen delivery and utilization by the tissues and organs, leading to hypoxia, acidosis, or organ failure. Therefore, this response is irrelevant and inaccurate.
Choice C) Shivering to generate heat is incorrect because this is not a result of hypothermia in the newborn, but rather a mechanism that is absent in them. Shivering is an involuntary contraction of the muscles that produces heat and raises the body temperature. It is a common response to cold exposure in adults and older children, but not in newborns. Newborns do not have the ability to shiver, as their muscles are immature and lack glycogen stores.
Instead, they rely on other methods to generate heat, such as non-shivering thermogenesis, which involves burning brown fat in certain areas of the body. Therefore, this response is irrelevant and inaccurate.
Choice D) Increased glucose demands is correct because this is a result of hypothermia in the newborn that can cause complications. Glucose demand is the amount of glucose that the body needs to produce energy and maintain its functions. Newborns have a high glucose demand, which helps them to support their metabolic rate and thermoregulation. However, some factors can increase the glucose demand of newborns, such as hypothermia, stress, or infection. A high glucose demand can deplete the glucose stores and cause hypoglycemia, which is a low level of glucose in the blood that can lead to seizures, brain damage, or death. Therefore, this response is clear and accurate.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
