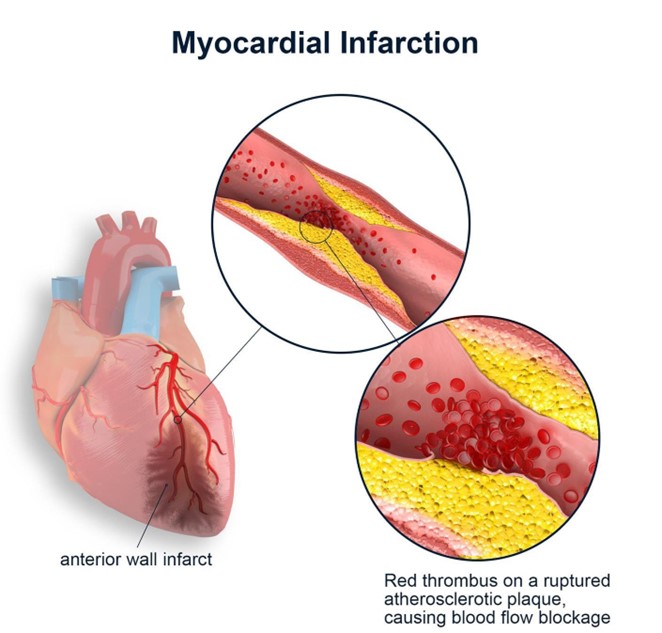
A nurse is admitting a client who has acute heart failure following myocardial infarction (MI). The nurse recognizes that which of the following prescriptions by the provider requires clarification?
Laboratory testing of serum potassium upon admission
Bumetanide 1 mg IV bolus every 12 hr
0.9% normal saline IV at 50 mL/hr continuous
Morphine sulfate 2 mg IV bolus every 2 hr PRN pain
The Correct Answer is C
Choice A Reason: This choice is incorrect because laboratory testing of serum potassium upon admission is an appropriate prescription for a client who has acute heart failure following MI. Serum potassium is an electrolyte that affects the cardiac function and rhythm. A normal serum potassium range is 3.5 to 5 mEq/L, and an abnormal level can indicate hypokalemia or hyperkalemia, which can cause arrhythmias, muscle weakness, or paralysis. Therefore, monitoring serum potassium is important to detect and correct any electrolyte imbalance and prevent complications.
Choice B Reason: This choice is incorrect because bumetanide 1 mg IV bolus every 12 hr is an appropriate prescription for a client who has acute heart failure following MI. Bumetanide is a loop diuretic that helps to reduce fluid retention and edema by increasing the urine output and sodium excretion. It may be used for clients who have heart failure, hypertension, or renal impairment, but it can cause hypokalemia, hypotension, or dehydration.
Therefore, administering bumetanide as prescribed can help to improve the cardiac output and reduce the preload and afterload.
Choice C Reason: This choice is correct because 0.9% normal saline IV at 50 mL/hr continuous is an inappropriate prescription for a client who has acute heart failure following MI. 0.9% normal saline is an isotonic solution that contains the same concentration of solutes as blood plasma. It may be used for clients who have fluid loss, dehydration, or shock, but it can worsen fluid overload and pulmonary edema in clients who have acute heart failure. Therefore, clarifying this prescription with the provider is necessary to prevent further deterioration of the client's condition.
Choice D Reason: This choice is incorrect because morphine sulfate 2 mg IV bolus every 2 hr PRN pain is an appropriate prescription for a client who has acute heart failure following MI. Morphine sulfate is an opioid analgesic that helps to relieve pain and anxiety by binding to the opioid receptors in the brain and spinal cord. It may be used for clients who have moderate to severe pain, dyspnea, or chest discomfort, but it can cause respiratory depression, hypotension, or nausea. Therefore, administering morphine sulfate as prescribed can help to reduce the oxygen demand and improve the cardiac function.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
Choice A Reason: This is correct because using log rolling to reposition the client helps maintain the alignment of the head and neck, which prevents further increases in ICP.
Choice B Reason: This is incorrect because placing a warming blanket on the client can cause vasodilation and increase cerebral blood flow, which can raise ICP.
Choice C Reason: This is incorrect because instructing the client to cough and deep breathe can increase intrathoracic pressure and impede venous return, which can elevate ICP.
Choice D Reason: This is incorrect because placing the client in a supine position can decrease cerebral perfusion pressure and increase ICP. The client should be placed in a semi-Fowler's position with the head elevated at 30 degrees.
Correct Answer is B
Explanation
Choice A Reason: This choice is incorrect because furosemide is a diuretic that helps to reduce fluid retention and edema. It may be used for clients who have heart failure or hypertension, but it does not treat pulmonary embolism.
Choice B Reason: This choice is correct because heparin is an anticoagulant that helps to prevent blood clots from forming or growing larger. It may be used for clients who have pulmonary embolism, which is a blockage of a pulmonary artery by a blood clot that usually originates from a deep vein thrombosis (DVT). Heparin can reduce the risk of complications such as pulmonary infarction or death.
Choice C Reason: This choice is incorrect because dexamethasone is a corticosteroid that helps to reduce inflammation and immune response. It may be used for clients who have allergic reactions, asthma, or autoimmune diseases, but it does not treat pulmonary embolism.
Choice D Reason: This choice is incorrect because epinephrine is a sympathomimetic that helps to stimulate the heart and blood vessels. It may be used for clients who have cardiac arrest, anaphylaxis, or severe asthma, but it does not treat pulmonary embolism.
Choice E Reason: This choice is incorrect because atropine is an anticholinergic that helps to block the effects of acetylcholine on the heart and smooth muscles. It may be used for clients who have bradycardia, atrioventricular block, or organophosphate poisoning, but it does not treat pulmonary embolism.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
