A nurse is assessing a patient with a surgical wound healing by secondary intention. Which finding should the nurse report to the charge nurse?
The wound is tender to touch.
The wound has a halo of erythema on the surrounding skin.
The wound is draining serosanguineous fluid.
The wound has pink, shiny tissue with a granular appearance.
The Correct Answer is B
Choice A rationale:
Tenderness to touch is a common finding in wounds healing by secondary intention. It's often due to inflammation, which is a normal part of the healing process. The inflammation brings in cells and substances that promote healing. However, increased tenderness, especially when accompanied by other signs of infection, should be reported.
Choice B rationale:
A halo of erythema on the surrounding skin is a sign of infection. This is a serious complication that can delay healing and lead to further complications. The erythema indicates that the infection is spreading beyond the wound edges and needs prompt attention.
Choice C rationale:
Drainage of serosanguineous fluid is also common in wounds healing by secondary intention. This fluid is a mixture of serum (clear yellowish fluid) and blood. It's a sign that the wound is cleaning itself and new tissue is forming. While excessive drainage or a change in color or odor could signal a problem, drainage itself is not necessarily a cause for concern.
Choice D rationale:
Pink, shiny tissue with a granular appearance is a sign of healthy granulation tissue. This is a type of tissue that forms during the healing process. It's rich in blood vessels and collagen, which are essential for wound healing. The presence of granulation tissue indicates that the wound is healing well.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
Choice A rationale:
Intractable pain is pain that is persistent and does not respond to usual pain management methods. While angina can be intractable in some cases, it does not typically manifest as pain in the arm and jaw. Moreover, the patient in this scenario has not yet undergone pain management efforts, so it's premature to classify the pain as intractable.
Choice B rationale:
Phantom pain is pain that is felt in a part of the body that has been amputated or is no longer there. The patient in this scenario has not experienced any amputations, so phantom pain is not a valid explanation for the arm and jaw pain.
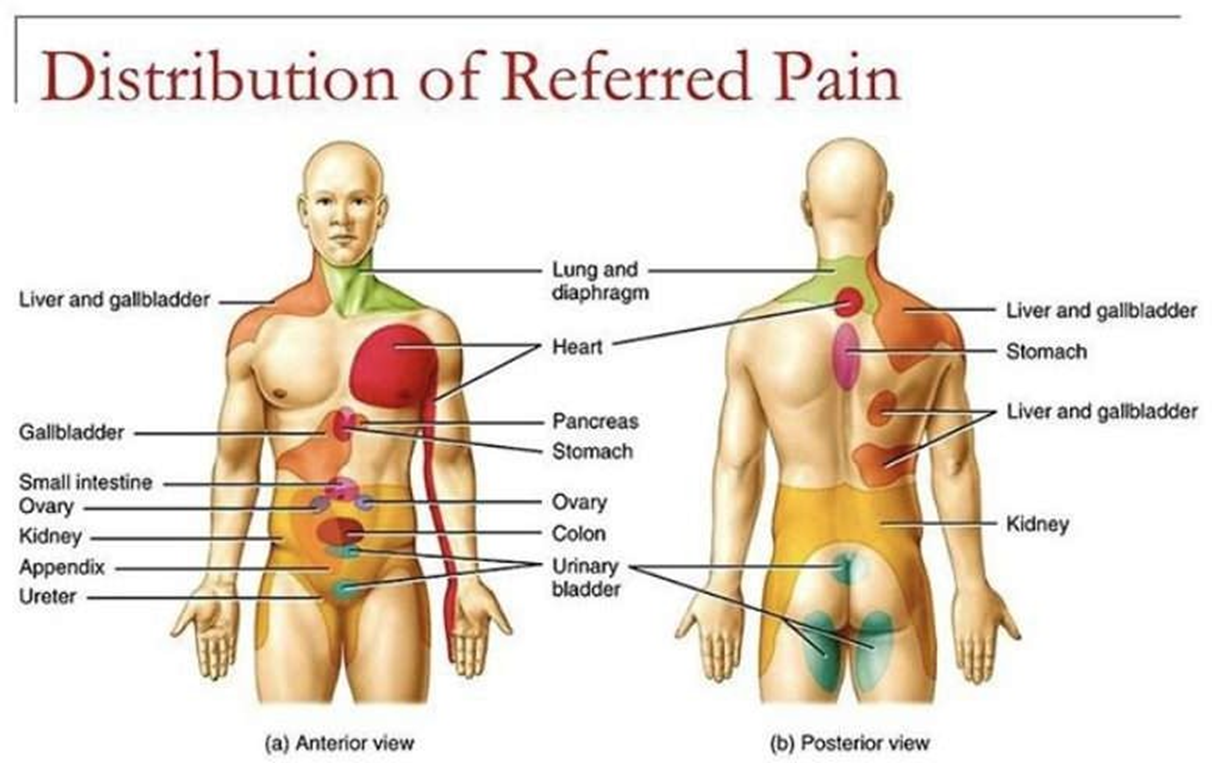
Choice C rationale:
Referred pain is pain that is felt in a part of the body that is different from the source of the pain. This is the most likely explanation for the arm and jaw pain in this patient. The heart and the arm and jaw share nerve pathways, so pain signals from the heart can be misinterpreted by the brain as coming from these other areas. This is a common phenomenon in patients with angina.
Choice D rationale:
Cramping pain is a type of pain that is often described as a muscle tightening or squeezing sensation. It is not typically associated with angina. While angina can sometimes cause chest tightness, it's not characterized by cramping in the arm and jaw.
Correct Answer is B
Explanation
Choice B rationale:
Stridor is a high-pitched, whistling sound that is heard during inspiration. It is a sign of upper airway obstruction, indicating a potentially life-threatening complication that requires immediate intervention.
Here's a detailed explanation of why stridor is the most concerning finding and why the other choices are not as indicative of a serious problem:
Stridor:
Mechanism: Stridor occurs when there is narrowing or obstruction of the upper airway, typically at the level of the larynx or trachea. This narrowing can be caused by various factors, including:
Laryngospasm: A sudden constriction of the vocal cords, often triggered by irritation or inflammation. Post-extubation edema: Swelling of the tissues in the airway after removal of the endotracheal tube.
Mucus plugging: Accumulation of thick secretions in the airway, which can partially block airflow.
Vocal cord dysfunction: Impairment of the vocal cords' movement, which can affect their ability to open and close properly.
Significance: Stridor is a serious sign because it indicates that airflow is significantly restricted. If left untreated, upper airway obstruction can lead to hypoxia (low oxygen levels) and respiratory failure.
Nursing intervention: If stridor is present, the nurse should immediately notify the provider and prepare for potential interventions to secure the airway, such as:
Reintubation: Reinserting the endotracheal tube to bypass the obstruction.
Nebulized racemic epinephrine: Medication to reduce swelling in the airway.
Heliox: A mixture of helium and oxygen that can improve airflow through a narrowed airway. Steroids: Medications to reduce inflammation in the airway.
Crackles (Choice A):
Description: Crackles are rattling, crackling sounds heard in the lungs, often during inspiration. They are typically associated with lower airway problems, such as pneumonia or pulmonary edema.
Significance: While crackles can indicate respiratory issues, they are not as immediately concerning as stridor in the context of post-extubation care.
Strong cough (Choice C):
Significance: A strong cough is generally a positive sign after extubation, as it indicates that the patient is able to clear secretions from their airway effectively.
Deep breathing (Choice D):
Significance: Deep breathing is also a positive sign, as it promotes lung expansion and oxygenation.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
