A nurse is caring for a client who had an evacuation of a subdural hematoma. Which of the following actions should the nurse take first?
Observe for cerebrospinal fluid (CSF) leaks from the evacuation site.
Check the oximeter.
Assess for an increase in temperature.
Monitor for manifestations of increased intracranial pressure.
The Correct Answer is B
Choice A Reason: Observing for cerebrospinal fluid (CSF) leaks from the evacuation site is important, but not the first action that the nurse should take. CSF leaks can indicate a breach in the dura mater, which can increase the risk of infection and meningitis. The nurse should inspect the dressing and the nose and ears for any clear or bloody drainage, and report any findings to the provider. However, these measures are secondary to ensuring adequate oxygenation and perfusion.
Choice B Reason: The first action the nurse should take when caring for a client post-evacuation of a subdural hematoma is to check the oximeter to ensure adequate oxygenation. Maintaining proper oxygenation is a priority because hypoxia and hypercapnia can lead to cerebral vasodilation, increasing intracranial pressure (ICP) and worsening neurological outcomes. Key Concept: Always prioritize Airway, Breathing, and Circulation (ABCs) when determining the most immediate nursing intervention.
Choice C Reason: Assessing for an increase in temperature is another important action, but not the first one that the nurse should take. An increase in temperature can indicate an infection, inflammation, or damage to the hypothalamus, which can affect the thermoregulation of the body. The nurse should monitor the temperature and administer antipyretics as prescribed. However, these measures are secondary to ensuring adequate oxygenation and perfusion.
Choice D Reason:This is crucial, but oxygenation status should be checked first since low oxygen levels can worsen ICP.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
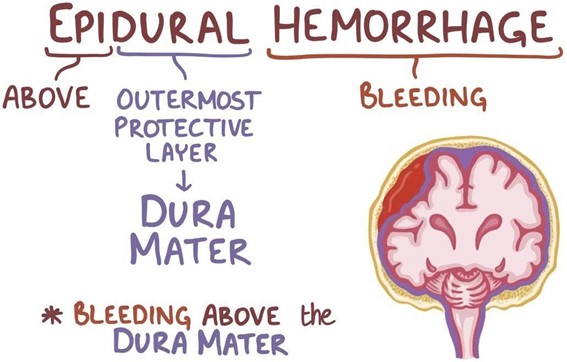
Choice A: Drainage of clear fluid from the ears is not an expected finding for a client who has an epidural hematoma, but rather a sign of a basilar skull fracture, which is a different type of head injury. The clear fluid is cerebrospinal fluid (CSF), which leaks from the brain through the fractured skull.
Choice B: Alternating periods of alertness and unconsciousness is an expected finding for a client who has an epidural hematoma, because it indicates a rapid increase in intracranial pressure (ICP) due to bleeding between the dura mater and the skull. The client may have a brief loss of consciousness at the time of injury, followed by a lucid interval, and then a rapid deterioration of mental status.
Choice C: Narrowing pulse pressure is not an expected finding for a client who has an epidural hematoma, but rather a sign of increased ICP due to any cause. Pulse pressure is the difference between systolic and diastolic blood pressure. As ICP rises, it compresses the brainstem and causes bradycardia and hypertension, resulting in a decreased pulse pressure.
Choice D: Extensive bruising in the mastoid area is not an expected finding for a client who has an epidural hematoma, but rather a sign of a basilar skull fracture, which is a different type of head injury. The bruising is also known as Batle's sign, and it occurs due to blood pooling behind the ear.
Correct Answer is D
Explanation
Choice A Reason: This is incorrect because administering a nitrate antihypertensive is not the first action, as it may cause a rapid drop in blood pressure and worsen the client's condition.
Choice B Reason: This is incorrect because obtaining the client's heart rate is not the first action, as it does not address the cause of autonomic dysreflexia or relieve the symptoms.
Choice C Reason: This is incorrect because assessing the client for bladder distention is not the first action, as it may take time and delay the treatment of autonomic dysreflexia.
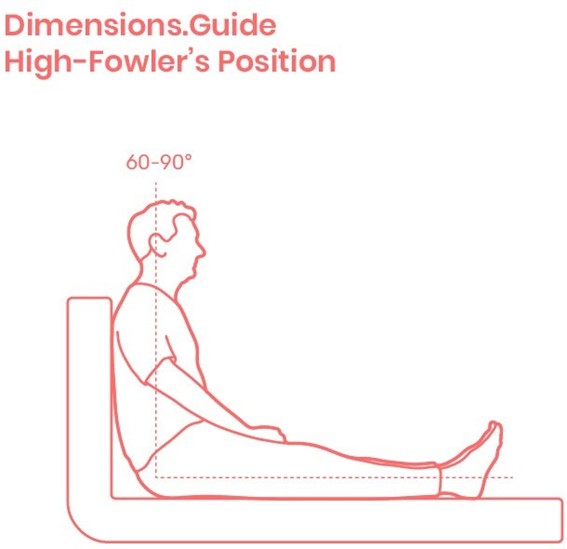
Choice D Reason: This is correct because placing the client in a high-Fowler's position is the first action, as it lowers the blood pressure by promoting venous return and reducing cardiac preload.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
