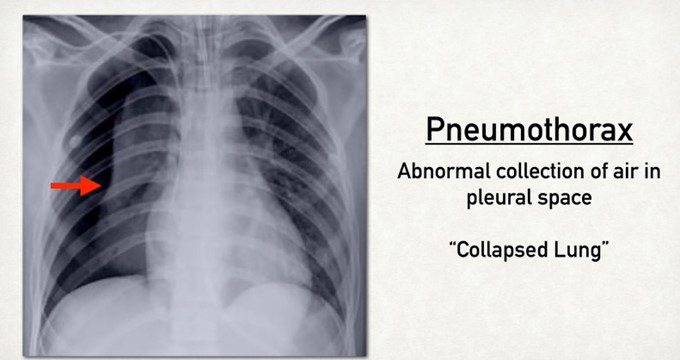
A nurse is monitoring a client who has a chest tube in place connected to wall suction due to a right-sided pneumothorax. The client complains of chest burning. Which of the following actions should the nurse take?
Increase the client's wall suction.
Reposition the client.
Clamp the client's chest tube.
Strip the client's chest tube.
The Correct Answer is B
Repositioning the client is the appropriate action for the nurse to take, as chest burning may indicate that the chest tube is kinked, twisted, or compressed, which can impair drainage and ventilation. The nurse should gently move the client to a different position and check that the chest tube is not bent or occluded by clothing, bedding, or furniture. The nurse should also ensure that there are no dependent loops or coils in the tubing and that it is secured to prevent dislodgment.
a) Increasing the client's wall suction is not advisable, as it can cause increased negative pressure in the pleural space and lead to tension pneumothorax. Increasing the wall suction does not affect the patency of the chest tube or the drainage of air or fluid from the lung. The nurse should maintain the wall suction at the prescribed level and monitor for any changes in the suction chamber.
c) Clamping the client's chest tube is not advisable, as it can cause air or fluid accumulation in the pleural space and lead to tension pneumothorax. Clamping the chest tube does not relieve chest burning or improve drainage or ventilation. The nurse should only clamp the chest tube for a brief period of time and under specific circumstances, such as changing the drainage system, assessing for an air leak, or preparing for chest tube removal.
d) Stripping the client's chest tube is not advisable, as it can cause increased negative pressure in the pleural space and lead to tissue damage or bleeding. Stripping the chest tube involves applying manual pressure along the tubing to force out any clots or debris that may obstruct drainage. However, this practice is not recommended, as it can cause more harm than good. The nurse should only milk the chest tube gently and intermittently if ordered by the provider and if there is evidence of obstruction.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is ["0.8"]
Explanation
To calculate the amount of mL to administer, the nurse should use the following formula:
(mg ordered / mg available) x mL available = mL to administer
Substituting the values from the question, the nurse should do the following:
(100 mg / 250 mg) x 2 mL = 0.8 mL

Correct Answer is B
Explanation
A humidifier bottle adds moisture to the oxygen, which prevents drying and irritation of the nasal mucosa
and enhances gas exchange.
a. Remove the nasal cannula while the client eats. This is not advisable, as the client may become hypoxic during eating, especially if they have pneumonia and impaired lung function. The nurse should monitor the client's oxygen saturation and respiratory status during meals and adjust the oxygen delivery device as needed.
c. Secure the oxygen tubing to the bed sheet near the client's head. This is not safe, as it can cause entanglement, dislodgement, or kinking of the tubing, which can compromise oxygen delivery and cause injury to the client.
d. Apply petroleum jelly to the nares as needed to soothe mucous membranes. This is not recommended, as petroleum products can ignite in the presence of oxygen and cause burns or fire. A water-based lubricant should be used instead.

Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
