A nurse in the ICU is caring for a client who has heart failure and is receiving a dobutamine drip. The nurse should identify that which of the following findings indicates that the medication is effective?
Increased urine output
Decreased blood glucose level
Decreased blood pressure
Increased heart rate
The Correct Answer is A
Choice A Reason: Dobutamine is a positive inotropic agent that increases the contractility of the heart and improves cardiac output. This leads to increased renal perfusion and urine output, which reduces the fluid overload and edema associated with heart failure. Therefore, this choice is correct.
Choice B Reason: Dobutamine does not have a direct effect on blood glucose level. It may cause hyperglycemia as a side effect, but this is not an indication of its effectiveness. Therefore, this choice is incorrect.
Choice C Reason: Dobutamine may cause a slight decrease in blood pressure due to vasodilation, but this is not its main therapeutic effect. A significant decrease in blood pressure may indicate hypovolemia, hypotension, or shock, which are adverse effects of dobutamine. Therefore, this choice is incorrect.
Choice D Reason: Dobutamine also has a positive chronotropic effect, which means it increases the heart rate. However, this is not a desired outcome for a client with heart failure, as it increases the oxygen demand of the heart and may worsen the condition. Therefore, this choice is incorrect.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
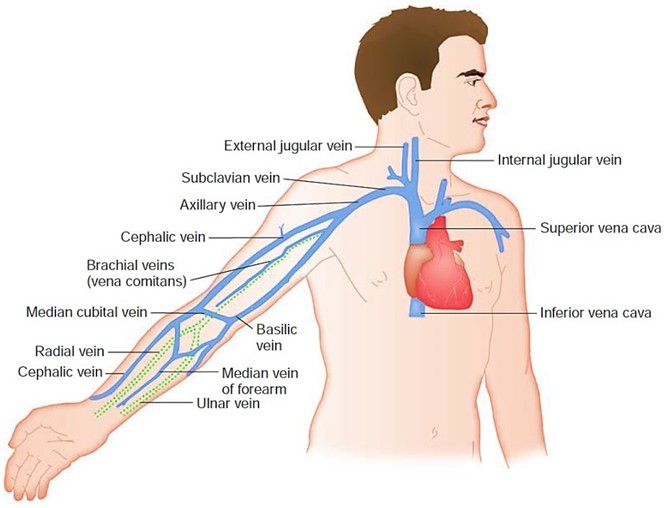
Choice A Reason: This choice is incorrect because inserting a central line is not a priority action for a client who has a sucking chest wound. A central line is a catheter that is inserted into a large vein in the neck, chest, or groin to administer fluids, medications, or blood products. It may be indicated for clients who have hypovolemia, sepsis, or shock, but it does not address the underlying cause of the client's respiratory distress.
Choice B Reason: This choice is incorrect because removing the dressing to inspect the wound may worsen the client's condition. A sucking chest wound is an open wound in the chest wall that allows air to enter and exit the pleural cavity with each breath. This creates a positive pressure in the pleural space that collapses the lung on the affected side and shifts the mediastinum to the opposite side, impairing the ventilation and circulation of both lungs. Therefore, the nurse should apply an occlusive dressing that covers three sides of the wound and allows air to escape but not enter the pleural cavity. Removing the dressing may allow more air to enter and increase the risk of tension pneumothorax, which is a life-threatening complication.
Choice C Reason: This choice is correct because administering oxygen via nasal cannula may help to improve the client's oxygenation and ventilation. A nasal cannula is a device that delivers oxygen through two prongs that fit into the nostrils. It can provide oxygen at low flow rates (1 to 6 L/min) and low concentrations (24 to 44 percent). The nurse should monitor the client's respiratory rate, pulse oximetry, and arterial blood gases to assess the effectiveness of oxygen therapy.
Choice D Reason: This choice is incorrect because raising the foot of the bed to a 90° angle may worsen the client's respiratory distress. This position may increase the pressure on the diaphragm and reduce the lung expansion. It may also decrease the venous return and cardiac output, leading to hypotension and shock. Therefore, the nurse should position the client in a semi-Fowler's position (30 to 45° angle) or high-Fowler's position (60 to 90° angle) to facilitate breathing and prevent further complications.

Correct Answer is B
Explanation
Choice A Reason: This choice is incorrect because administering a vasodilator medication may lower the blood pressure and worsen the cerebral perfusion. A vasodilator medication is a drug that relaxes the blood vessels and reduces the resistance to blood flow. It may be used for clients who have hypertension, angina, or heart failure, but it does not help to reduce the intracranial pressure (ICP).
Choice B Reason: This choice is correct because elevating the head of the bed to 30° may help to improve the venous drainage and decrease the ICP. ICP is the pressure exerted by the brain tissue, cerebrospinal fluid (CSF), and blood within the cranial cavity. A normal ICP range is 5 to 15 mm Hg, and an elevated ICP (>20 mm Hg) can cause cerebral ischemia, herniation, or death. Therefore, positioning the client in a semi-Fowler's position (30° angle) or high- Fowler's position (60° to 90° angle) can facilitate breathing and prevent further complications.
Choice C Reason: This choice is incorrect because applying a cold compress to the forehead may cause vasoconstriction and increase the ICP. A cold compress is a device that applies cold temperature to a body part to reduce inflammation, pain, or swelling. It may be used for clients who have headaches, sprains, or bruises, but it does not help to reduce the ICP.
Choice D Reason: This choice is incorrect because decreasing the oxygen flow rate may cause hypoxia and worsen the cerebral ischemia. Hypoxia is a condition in which the body or a part of it does not receive enough oxygen. It may cause symptoms such as confusion, agitation, or cyanosis. Therefore, providing adequate oxygenation and ventilation is essential to maintain the brain function and prevent further damage.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
