The nurse is caring for a postoperative client who has a chest tube connected to suction and a water seal drainage system. Which of the following indicates to the nurse that the chest tube is functioning properly?
Equal amount of fluid drainage in each collection chamber
Fluctuation of the fluid level within the water seal chamber
Continuous bubbling within the water seal chamber
Absence of fluid in the drainage tubing
The Correct Answer is B
Choice A Reason: Equal amount of fluid drainage in each collection chamber is not a sign of proper chest tube function. The amount of fluid drainage depends on the type and extent of the client's injury or surgery, and may vary from one chamber to another.
Choice B Reason: Fluctuation of the fluid level in the water seal chamber (tidaling) indicates that the chest tube is functioning properly. This fluctuation corresponds with the client's respirations and shows that air or fluid is being effectively removed from the pleural space.
Choice C Reason:Continuous bubbling within the water seal chamber: Continuous bubbling in the water seal chamber indicates an air leak, which is not normal unless the client has a pneumothorax and air is being evacuated. Otherwise, it suggests a problem with the system.
Choice D Reason: Absence of fluid in the drainage tubing is not a sign of proper chest tube function. It may indicate that the chest tube is obstructed, kinked, or clamped, or that the suction is not working properly. The nurse should assess and troubleshoot the chest tube system.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
Choice A Reason: This is incorrect because a client who is post-CABG and has high cholesterol is not in immediate danger, as atorvastatin is a long-term medication that lowers cholesterol and prevents cardiovascular complications.
Choice B Reason: This is incorrect because a client who has pneumonia and a slightly elevated WBC count is not in immediate danger, as piperacillin is an antibiotic that treats bacterial infections.
Choice C Reason: This is correct because a client who has renal failure and a high serum potassium level is in immediate danger, as sodium polystyrene sulfonate is an emergency medication that lowers potassium and prevents cardiac arrhythmias.
Choice D Reason: This is incorrect because a client who has anemia and a mild hemoglobin deficiency is not in immediate danger, as epoetin alfa is a long-term medication that stimulates red blood cell production and improves oxygen delivery.
Correct Answer is A
Explanation
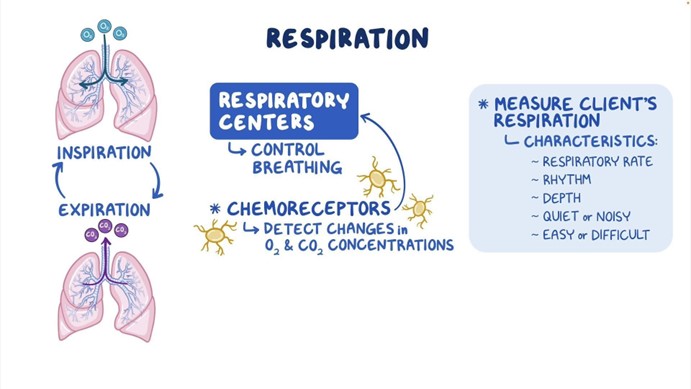
The correct answer is a. Respiratory status.
Choice A: Respiratory Status
Reason: After the evacuation of a subdural hematoma, monitoring the respiratory status is crucial. This is because changes in respiratory patterns can indicate increased intracranial pressure (ICP) or brainstem compression, which are life-threatening conditions. Ensuring that the airway is clear and that the patient is breathing adequately is the top priority. Normal respiratory rate for adults is 12-20 breaths per minute.
Choice B: Temperature
Reason: While monitoring temperature is important to detect infections or other complications, it is not the immediate priority in the acute postoperative period following a subdural hematoma evacuation. Fever can indicate infection, but it is less likely to cause immediate life-threatening complications compared to respiratory issues.
Choice C: Intracranial Pressure
Reason: Monitoring intracranial pressure (ICP) is very important in patients with brain injuries. Normal ICP ranges from 5-15 mmHg. However, changes in respiratory status can be an early indicator of increased ICP. Therefore, while ICP monitoring is critical, ensuring the patient’s respiratory status is stable takes precedence.
Choice D: Serum Electrolytes
Reason: Serum electrolytes are important to monitor for overall metabolic stability and to detect imbalances that could affect neurological function. Normal ranges for key electrolytes are: Sodium (135-145 mEq/L), Potassium (3.5-4.5 mEq/L), and Chloride (80-100 mEq/L). However, these are not the immediate priority in the acute phase following surgery compared to respiratory status.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
