A nurse is caring for a client who has dysphagia. Which of the following actions should the nurse take?
Place the client in a semi-Fowler's position when eating.
Initiate calorie count of daily food intake.
Instruct the client to keep their chin up when swallowing.
Provide food in a thin liquid consistency.
The Correct Answer is A
Place the client in a semi-Fowler's position when eating. The semi-Fowler's position involves elevating the head of the bed to an angle of 30 to 45 degrees. This position helps prevent aspiration by facilitating proper swallowing and reducing the risk of food or liquid entering the airway.

Initiating a calorie count of daily food intake is not a specific action for dysphagia. Calorie counting is generally used for monitoring caloric intake in clients with specific dietary needs or conditions, but it is not directly related to dysphagia management. The focus for dysphagia management is on ensuring safe swallowing and preventing complications such as aspiration.
Instructing the client to keep their chin up when swallowing is not appropriate for dysphagia management. This action can actually increase the risk of aspiration. The proper technique for swallowing with dysphagia typically involves tucking the chin slightly down towards the chest to help close off the airway and direct the food or liquid down the esophagus.
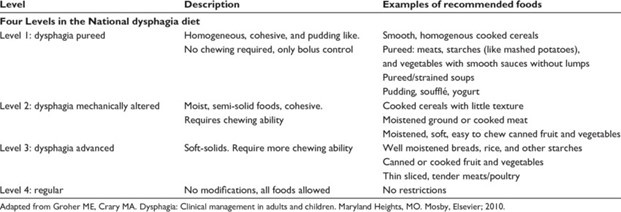
Providing food in a thin liquid consistency is not appropriate for dysphagia unless specifically recommended by a healthcare professional. Dysphagia diets typically involve modifying the consistency of food and liquids based on the client's swallowing abilities and recommendations from a speech-language pathologist or dietitian. Different levels of texture modifications (such as pureed, minced, or mechanically soft) may be prescribed to ensure safe swallowing and reduce the risk of aspiration.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
Limiting protein intake is an important dietary modification for clients with chronic kidney disease. High protein intake can increase the workload on the kidneys and lead to further decline in kidney function. Restricting protein intake helps reduce the accumulation of waste products in the blood, such as urea and creatinine, which are normally eliminated by the kidneys. The specific amount of protein restriction will depend on the stage of CKD and the client's individual needs. It is important for the client to work with a registered dietitian who specializes in kidney disease to determine the appropriate protein intake.
Limit calcium intake: Calcium intake does not need to be limited unless there are specific complications related to calcium metabolism, such as hypercalcemia or certain types of kidney stones. Calcium is important for bone health, and adequate intake should be maintained unless otherwise directed by the healthcare provider.
Increase potassium intake: In most cases of chronic kidney disease, potassium intake needs to be limited. Damaged kidneys may have difficulty regulating potassium levels, and high levels of potassium in the blood can be dangerous. The client should be instructed to limit potassium intake and avoid high-potassium foods, such as bananas, oranges, tomatoes, and potatoes, unless specifically advised otherwise by their healthcare provider.
Increase phosphorus intake: Phosphorus intake needs to be restricted in chronic kidney disease, especially in later stages. Elevated levels of phosphorus in the blood can lead to bone and cardiovascular complications. The client should be educated on foods that are high in phosphorus, such as dairy products, nuts, and cola drinks, and instructed to limit their intake
Correct Answer is C
Explanation
A level 1 dysphagia diet, also known as a pureed diet, is recommended for individuals with severe swallowing difficulties. It involves pureeing or blending all foods to a smooth consistency to facilitate swallowing and prevent choking.
● Chicken noodle soup: This option typically contains solid ingredients such as chicken, noodles, and vegetables, which are not suitable for a level 1 dysphagia diet. The client may have difficulty swallowing these solid components.
● Apple juice: Liquids, including apple juice, are generally not included in a level 1 dysphagia diet as they require minimal swallowing effort. However, it is essential to consult a speech-language pathologist or dysphagia specialist regarding the client's specific liquid consistency recommendations.
● Pudding: Pudding is an ideal choice for a level 1 dysphagia diet as it can be easily pureed to a smooth consistency that is safe for swallowing. It provides a creamy and soft texture that is easier for individuals with dysphagia to manage.
● Milk: Milk is not typically recommended for a level 1 dysphagia diet as it is a liquid and requires minimal swallowing effort. Similar to apple juice, specific liquid consistency recommendations should be sought from a dysphagia specialist.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
