A nurse is caring for a client who has peripheral arterial disease (PAD). Which of the following symptoms should the nurse expect to find in the early stage of the disease?
Dependent rubor
Intermitent claudication
Foot ulcers
Rest pain
The Correct Answer is B
The correct answer is B
Choice B reason: Intermittent claudication
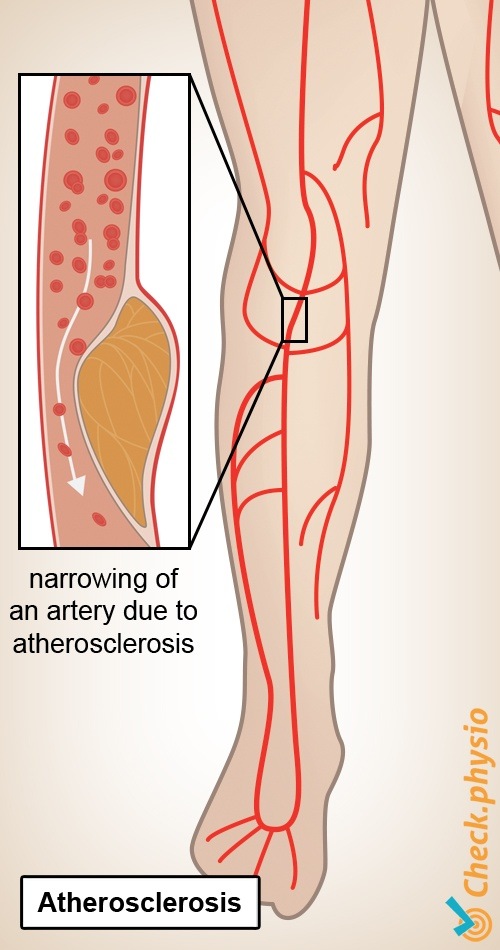
Intermittent claudication is a characteristic symptom of PAD in the early stage, due to the reduced blood flow to the muscles during exercise. It is a cramping pain in the legs that occurs with walking and is relieved by rest.
Choice A reason: Dependent rubor is a sign of PAD in the advanced stage, due to the impaired vasodilation and reactive hyperemia. It is a reddish color of the lower extremities that occurs when they are lowered and disappears when they are elevated.
Choice C reason: Foot ulcers are a complication of PAD in the late stage, due to the poor wound healing and tissue necrosis. They are usually located on the toes, heels, or pressure points.
Choice D reason: Rest pain is another sign of PAD in the late stage, due to the severe ischemia and nerve damage. It is a persistent pain in the feet or toes that occurs at night and is not relieved by rest.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
A: Vertigo is a common finding in clients with essential hypertension due to changes in blood flow and possible impacts on the inner ear, which can affect balance.
B: Blurred vision, while it can be associated with hypertension, is not as directly related to essential hypertension as vertigo is. It is more commonly a sign of complications from prolonged uncontrolled hypertension.
C: Dyspnea or difficulty breathing is not typically a direct symptom of essential hypertension, though it can be a symptom of complications such as heart failure, which can be a result of long-standing, uncontrolled hypertension.
D: Uremia, which is an elevated level of waste products in the blood, is not a symptom of essential hypertension but rather a sign of kidney failure, which can be a secondary complication of chronic hypertension. Essential hypertension itself does not directly cause uremia.
Correct Answer is B
Explanation
Right-sided heart failure is a condition in which the right ventricle fails to pump blood effectively to the lungs, causing a backup of blood in the systemic circulation. This leads to increased pressure in the right atrium and the vena cava, which can be measured by the central venous pressure (CVP). A normal CVP is 2 to 6 mm Hg, but in right-sided heart failure, it can rise above 10 mm Hg. Symptoms of right-sided heart failure include peripheral edema, jugular venous distension, hepatomegaly, ascites, and weight gain.
a. Increased pulmonary artery wedge pressure (PAWP). This statement is incorrect because it describes a finding of left-sided heart failure, not right-sided heart failure. Left-sided heart failure is a condition in which the left ventricle fails to pump blood effectively to the systemic circulation, causing a backup of blood in the pulmonary circulation. This leads to increased pressure in the left atrium and the pulmonary capillaries, which can be measured by the pulmonary artery wedge pressure (PAWP). A normal PAWP is 6 to 12 mm Hg, but in left-sided heart failure, it can rise above 18 mm Hg. Symptoms of left-sided heart failure include dyspnea, orthopnea, paroxysmal nocturnal dyspnea, crackles in the lungs, and pink frothy sputum.
c. Decreased brain natriuretic peptide (BNP). This statement is incorrect because it describes a finding of normal or reduced cardiac function, not heart failure. Brain natriuretic peptide (BNP) is a hormone secreted by the cardiac cells in response to increased stretch and pressure in the ventricles. It acts as a diuretic and a vasodilator, lowering blood volume and blood pressure. BNP is used as a biomarker for diagnosing and monitoring heart failure, as it reflects the degree of ventricular dysfunction. A normal BNP level is less than 100 pg/mL, but in heart failure, it can rise above 400 pg/mL.
d. Decreased specific gravity. This statement is incorrect because it describes a finding of dilute urine, not concentrated urine. Specific gravity is a measure of the concentration of solutes in urine, reflecting the ability of the kidneys to regulate fluid balance. A normal specific gravity is 1.005 to 1.030, but it can vary depending on fluid intake and output, hydration status, and renal function. In right-sided heart failure, fluid retention and reduced renal perfusion can cause oliguria and increased specific gravity of urine.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
