A nurse is caring for a client who has ulcerative colitis and is teaching the client about the common link with Crohn's disease. Which of the following information should the nurse include?
Both are inflammatory.
Both affect the entire alimentary canal.
Both will require a bowel diversion.
Both disorders are caused by low-fat, high-fiber diets.
The Correct Answer is A
Choice A reason: This is the correct answer because both ulcerative colitis and Crohn's disease are inflammatory bowel diseases (IBD) that cause chronic inflammation of the digestive tract. The inflammation can cause symptoms such as abdominal pain, diarrhea, bleeding, weight loss, or fever. The nurse should educate the client on how to manage inflammation and prevent complications.
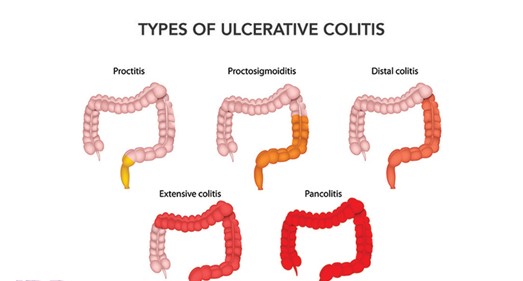
Choice B reason: This is incorrect because both ulcerative colitis and Crohn's disease do not affect the entire alimentary canal, but different parts of it. Ulcerative colitis affects only the colon (large intestine) and rectum, while Crohn's disease can affect any part of the digestive tract from mouth to anus, most commonly the ileum (the last part of the small intestine). The nurse should explain the differences in location and extent of
the diseases.
Choice C reason: This is incorrect because both ulcerative colitis and Crohn's disease do not always require a bowel diversion, but only in some cases. A bowel diversion is a surgical procedure that creates an opening (stoma) in the abdomen to divert fecal matter into an external bag or pouch. It may be done to treat severe complications such as perforation, obstruction, fistula, or cancer. The nurse should inform the client about the indications, types, and care of bowel diversions.
Choice D reason: This is incorrect because both ulcerative colitis and Crohn's disease are not caused by low-fat, high-fiber diets, but by unknown factors. The exact causes of IBD are not clear, but they may involve genetic, immune, environmental, or microbial factors. Low-fat, high-fiber diets may help prevent or reduce symptoms of IBD, but they do not cause them. The nurse should advise the client on how to follow a balanced and nutritious diet that suits their individual needs and preferences.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
Choice A Reason: This is incorrect because inability to recognize any words may indicate a problem with the auditory cortex, which is the part of the brain that processes sound, not the inner ear. The inner ear consists of the cochlea, which converts sound waves into nerve impulses, and the vestibular system, which helps with balance and orientation.
Choice B Reason: This is correct because loss of balance is a common symptom of an inner ear infection. An inner ear infection can cause inflammation and fluid buildup in the vestibular system, which can disrupt the sense of equilibrium and cause vertigo, dizziness, or nausea.
Choice C Reason: This is incorrect because twitching of the cheek may indicate a problem with the facial nerve, which controls the muscles of facial expression, not the inner ear. The facial nerve runs close to the inner ear, but it is not part of it.
Choice D Reason: This is incorrect because lack of air sound may indicate a problem with the outer or middle ear, which transmit sound waves to the inner ear, not the inner ear itself. The outer ear consists of the pinna and the ear canal, and the middle ear consists of the eardrum and the ossicles.
Correct Answer is C
Explanation
Choice A Reason: This is correct because incorporating foods rich in vitamin C in the diet can help prevent or delay macular degeneration. Vitamin C is an antioxidant that can protect the cells of the macula, which is the central part of the retina that is responsible for sharp and detailed vision, from oxidative stress and damage. The nurse should also advise the client to consume foods rich in other antioxidants, such as vitamin E, zinc, lutein, and zeaxanthin.
Choice B Reason: This is correct because receiving injections into the eye can help treat macular degeneration. Injections are a form of anti-vascular endothelial growth factor (anti-VEGF) therapy, which can block abnormal blood vessel growth and leakage in the macula that can cause vision loss. The nurse should explain to the client how often and how long they need to receive injections and what side effects or complications they may experience.
Choice C Reason: This is incorrect because vision will not be restored after using eye drops for macular degeneration. Eye drops are not a proven or effective treatment for macular degeneration, which is a chronic and progressive condition that causes irreversible vision loss. The nurse should reinforce education by informing the client that eye drops may only provide temporary relief of dryness or irritation, but they will not improve or restore vision.
Choice D Reason: This is correct because vision will become progressively more blurry with macular degeneration. Macular degeneration can cause blurred or distorted central vision, difficulty reading or recognizing faces, or dark spots in the visual field. The nurse should educate the client on how to cope with vision loss and use adaptive devices, such as magnifiers, large-print books, or voice-activated technology.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
