A nurse is caring for an adolescent client who has cystic fibrosis. Which of the following actions should the nurse instruct the client to take prior to initiating postural drainage?
Complete oral hygiene.
Use an ibuterol inhaler.
Take pancrelipase.
Eat a meal.
The Correct Answer is B
The correct answer is B.
Choice A reason: Completing oral hygiene is important for overall health, especially for individuals with cystic fibrosis, as they are at a higher risk for dental problems due to thick mucus that can harbor bacteria. However, oral hygiene does not have a direct impact on the effectiveness of postural drainage. Postural drainage is a technique used to clear mucus from the lungs, and while maintaining oral hygiene is beneficial, it is not a prerequisite for this procedure.
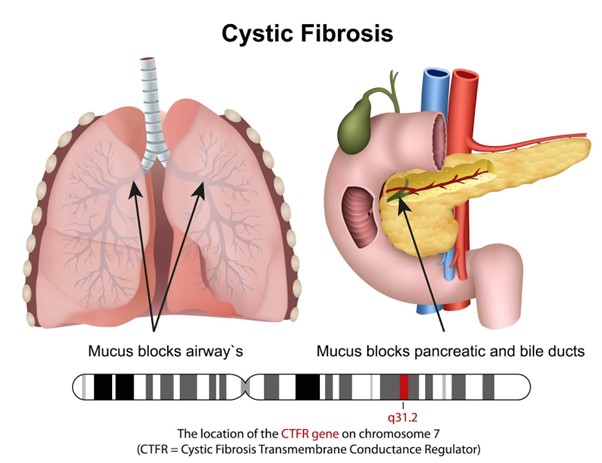
Choice B reason: Using a bronchodilator, such as an ibuterol inhaler, is recommended before postural drainage because it helps to open the airways, making the procedure more effective. Bronchodilators work by relaxing the muscles around the airways, which can become constricted in conditions like cystic fibrosis. This relaxation allows for easier clearance of mucus during postural drainage.
Choice C reason: Pancrelipase is an enzyme supplement used to aid digestion in patients with cystic fibrosis, who often have pancreatic insufficiency. While taking pancrelipase is crucial for nutrient absorption, it is not specifically related to the respiratory treatment of postural drainage. Therefore, it is not necessary to take pancrelipase immediately before this procedure.
Choice D reason: Eating a meal before postural drainage is not recommended. The procedure involves placing the body in positions that facilitate the drainage of mucus from the lungs due to gravity. Having a full stomach can cause discomfort, increase the risk of vomiting, and may hinder the effectiveness of the drainage. It is best to perform postural drainage when the stomach is empty, either before meals or at least 1.5 hours after eating.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation

Wound dehiscence can lead to infection, bleeding, and evisceration (protrusion of internal organs through the incision). The nurse should report this finding to the provider immediately and cover the wound with a sterile dressing moistened with sterile saline solution.
Choice A is wrong because mild swelling under the sutures near the incisional line is a normal finding in the early stages of wound healing. It does not indicate infection or dehiscence unless accompanied by other signs such as redness, warmth, pain, or purulent drainage.
Choice B is wrong because crusting of exudate on the incisional line is also a normal finding that indicates the formation of a scab.
A scab protects the wound from infection and helps it heal faster. The nurse should not remove the scab unless instructed by the provider.
Choice D is wrong because pink-tinged coloration on the incisional line is another normal finding that shows healthy granulation tissue.
Granulation tissue is new tissue that fills in the wound and helps it close. It is usually pink or red and moist.
The nurse should follow these general tips for postoperative abdominal incision care:
- Always wash your hands before and after touching your incisions.
- Inspect your incisions and wounds every day for signs your healthcare provider has told you are red flags or concerning.
- Look for any bleeding.
If the incisions start to bleed, apply direct and constant pressure to the incisions.
- Avoid wearing tight clothing that might rub on your incisions.
- Try not to scratch any itchy wounds.
- You can shower starting 48 hours after your operation but no scrubbing or soaking of the abdominal wounds in a tub.
- After the initial dressing from the operating room is removed, you can leave the wound open to air unless there is drainage or you feel more comfortable with soft gauze covering the wound.
- Surgical glue (Indermil) will fall off over a period of up to 2-3 weeks.
Do not put any topical ointments or lotions on the incisions.
- Do not rub over the incisions with a washcloth or towel.
- No tub baths, hot tubs, or swimming until evaluated at your clinic appointment.
Correct Answer is C
Explanation
The correct answer is c. Document the client's behavior prior to being placed in seclusion.
Rationale for Choice a. Discuss with the client his inappropriate behavior prior to seclusion:
While discussing the client's behavior may be helpful in some situations, it is not the most appropriate action to take immediately before seclusion. This is because:
- Escalation:Attempting to discuss behavior in the moments leading up to seclusion can potentially escalate the situation and further jeopardize the safety of the client,staff,and other patients.
- Impaired Insight:Clients requiring seclusion may have limited ability to engage in rational discussion due to heightened emotional states,cognitive impairment,or acute mental illness.
- Limited Receptiveness:The client may not be receptive to feedback or discussion while in a state of crisis,potentially leading to frustration and further agitation.
Rationale for Choice b. Offer fluids every 2 hr.:
Offering fluids is a basic nursing intervention, but it is not the priority action in this scenario. The primary focus at this time is ensuring safety and managing the acute behavioral crisis. Addressing hydration needs can be attended to after the client is safely placed in seclusion.
Rationale for Choice d. Assess the client’s behavior once every hour.:
Regular assessment is crucial, but hourly assessment is not frequent enough in this situation. Clients in seclusion require close monitoring and assessment at more frequent intervals to ensure their safety and well-being, as well as to evaluate the effectiveness of the seclusion intervention.
Rationale for Choice c. Document the client’s behavior prior to being placed in seclusion.:
This is the most appropriate action for the nurse to take for the following reasons:
- Legal and Ethical Requirements:Accurate documentation of the client's behavior prior to seclusion is essential for legal and ethical reasons.It serves as a record of the rationale for seclusion,supporting the decision-making process and ensuring adherence to best practices and patient rights.
- Assessment and Intervention Planning:Detailed documentation provides valuable information for ongoing assessment and intervention planning.It allows healthcare professionals to track the client's progress,identify patterns in behavior,and make informed decisions about the continuation or discontinuation of seclusion.
- Communication and Collaboration:Comprehensive documentation facilitates effective communication and collaboration among the healthcare team members,ensuring continuity of care and promoting a holistic approach to the client's treatment.
- Evaluation and Quality Improvement:Accurate documentation enables evaluation of the effectiveness of seclusion interventions and contributes to quality improvement initiatives within the healthcare setting.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
