A nurse is conducting an in-service program for a group of nurses working at the women's health facility about the causes of spontaneous abortion. The nurse determines that the teaching was successful when the group identifies which condition as the most common cause of first trimester abortions?
Cervical insufficiency
Uterine fibroids
Fetal genetic abnormalities
Maternal disease
The Correct Answer is C
Choice A Reason: This is incorrect because cervical insufficiency is a condition where the cervix dilates prematurely and painlessly during pregnancy, leading to preterm delivery or second trimester abortion. It is not a common cause of first trimester abortion, which occurs before 12 weeks of gestation.
Choice B Reason: This is incorrect because uterine fibroids are benign tumors that grow in or on the uterus. They may cause heavy bleeding, pain, or infertility, but they are not a common cause of first trimester abortion. They may increase the risk of miscarriage in later stages of pregnancy.
Choice C Reason: This is correct because fetal genetic abnormalities are the most common cause of first trimester abortion, accounting for up to 70% of cases. Fetal genetic abnormalities are errors in the number or structure of chromosomes that occur during fertilization or cell division. They can cause developmental defects or fetal demise that result in spontaneous abortion.
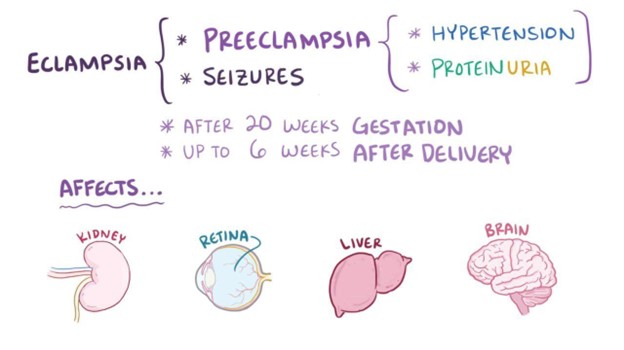
Choice D Reason: This is incorrect because maternal disease is not a common cause of first trimester abortion. Maternal disease refers to any medical condition that affects the mother's health or pregnancy outcome, such as diabetes, hypertension, thyroid disorders, or infections. Maternal disease may increase the risk of miscarriage in later stages of pregnancy or cause other complications such as preterm labor or preeclampsia.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is ["2"]
Explanation
The correct answer is 2 mL. To calculate the volume to administer, the nurse should use the following formula:
Volume (mL) = Dose (units) / Concentration (units/mL)
Plugging in the given values, we get:
Volume (mL) = 1,200,000 units / 600,000 units/mL
Volume (mL) = 2 mL
Rounding to the nearest whole number, we get 2 mL.

Correct Answer is D
Explanation
Choice A Reason: This is incorrect because ferrous sulfate is an iron supplement that is used to treat or prevent iron-deficiency anemia. It has no effect on magnesium sulfate, which is a medication that lowers blood pressure and prevents seizures in severe preeclampsia.
Choice B Reason: This is incorrect because potassium chloride is an electrolyte supplement that is used to treat or prevent low levels of potassium in the blood. It has no effect on magnesium sulfate, which can cause hypermagnesemia, or high levels of magnesium in the blood.
Choice C Reason: This is incorrect because calcium carbonate is an antacid that is used to treat or prevent heartburn, indigestion, or calcium deficiency. It has no effect on magnesium sulfate, which can cause hypocalcemia, or low levels of calcium in the blood.
Choice D Reason: This is correct because calcium gluconate is an antidote that is used to treat magnesium toxicity, which can occur when magnesium sulfate is given in high doses or for prolonged periods. Calcium gluconate reverses the effects of magnesium sulfate on the neuromuscular and cardiovascular systems, such as muscle weakness, respiratory depression, cardiac arrhythmias, or cardiac arrest.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
