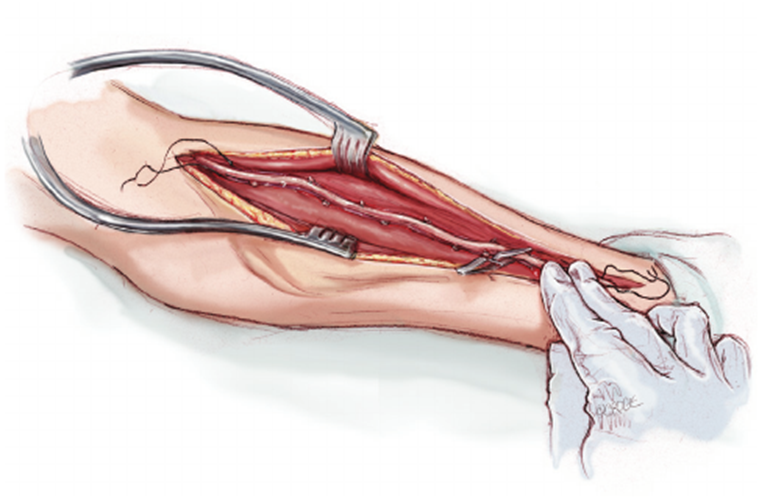
A nurse is planning care for a client who is postoperative following the insertion of an arteriovenous graft in their left forearm. Which of the following actions should the nurse include in the plan of care?
Check the pulse distal to the graft.
Keep the left forearm below the level of the heart.
Collect blood specimens from the graft.
Splint the left forearm to prevent damage to the graft.
The Correct Answer is A
Choice A reason: Checking the pulse distal to the graft is essential to ensure that the graft is patent and that there is adequate blood flow to the distal extremity. A palpable pulse indicates that the graft is functioning properly and not occluded. The absence of a pulse could signify a serious complication, such as thrombosis or stenosis, which requires immediate attention.
Choice B reason: Keeping the left forearm below the level of the heart is not recommended as it can increase venous pressure and swelling, potentially compromising graft function. The extremity should be kept at or above heart level to promote venous return and reduce the risk of edema.
Choice C reason: Collecting blood specimens from the graft is generally avoided to prevent damage to the graft. Blood draws can be performed from other sites to protect the integrity of the graft.
Choice D reason: Splinting the left forearm is not a standard postoperative care measure for an arteriovenous graft. While protecting the graft from injury is important, immobilization with a splint is not necessary and can impede mobility and circulation.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
Choice A reason: Cheyne-Stokes respirations, characterized by a pattern of irregular breathing with periods of apnea, can be a sign of brain stem compression due to increased intracranial pressure. However, it is not typically the first sign of deteriorating neurological status.
Choice B reason: Pupillary dilation, especially if it is unilateral, can indicate pressure on the cranial nerves due to increased intracranial pressure. It is a concerning sign but may not be the first to appear as neurological function deteriorates.
Choice C reason: An altered level of consciousness is often the first sign of deteriorating neurological status in a patient with increased intracranial pressure. Changes in consciousness can range from slight disorientation or confusion to complete unresponsiveness.
Choice D reason: Decorticate posturing, which involves abnormal flexion of the arms with extension of the legs, indicates significant brain injury and is a later sign of increased intracranial pressure, not typically the first sign.
Correct Answer is B
Explanation
Choice A reason: The statement "You should limit discussing past events with the client" does not necessarily incorporate the client's and family's cultural beliefs. Discussing past events can be a part of reminiscence therapy, which can be beneficial for clients with terminal illnesses. It allows them to reflect on their life experiences and can provide a sense of fulfillment or closure.
Choice B reason: Saying "We will respect what is important to you" is a broad and inclusive statement that acknowledges the importance of the client's and family's cultural beliefs. It implies that the care team is willing to listen and adapt the care plan to align with the client's values, which is a fundamental aspect of culturally competent care. This approach can help ensure that the client's end-of-life care is respectful and responsive to their individual needs.
Choice C reason: Offering to "arrange all burial services" may not be appropriate as it assumes that the family requires assistance with this aspect of care without first understanding their specific cultural or religious practices. It is important to have a conversation with the client and family about their preferences and needs regarding end-of-life rituals before making any arrangements.
Choice D reason: The statement "Grieving should not be done in front of the client" may not align with the cultural beliefs of the client and family. Grieving practices vary widely among different cultures, and some may find it important to express grief openly in the presence of the dying person. It is essential to respect and accommodate the family's grieving process.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
