A nurse is reinforcing teaching with a client who is at 34 weeks of gestation and at risk for placental abruption. Does the nurse recognize that which of the following is the most common risk factor for a placental abruption?
Maternal hypertension.
Maternal cocaine use.
Maternal cigarette smoking.
Maternal battering.
The Correct Answer is A
The correct answer is choice A, Maternal hypertension.
Choice A rationale:
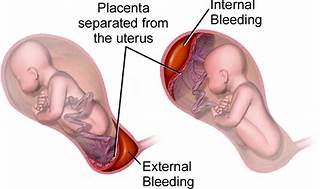
Maternal hypertension is widely recognized as the most common risk factor for placental abruption. High blood pressure can cause the placenta to detach from the uterine wall, leading to abruption. In summary, while all the listed factors can contribute to the risk of placental abruption, maternal hypertension stands out as the most common cause, supported by multiple health sources. It’s important for nurses to recognize and manage hypertension in pregnant clients to minimize the risk of this serious complication.
Choice B rationale:
While maternal cocaine use is a significant risk factor for placental abruption due to its vasoconstrictive effects, which can compromise the placental blood flow, it is not as common as maternal hypertension.
Choice C rationale:
Maternal cigarette smoking is also a risk factor for placental abruption. Smoking can lead to a variety of complications in pregnancy, including placental problems, but again, it is less common than hypertension as a cause for abruption.
Choice D rationale:
Maternal battering can lead to trauma which may result in placental abruption. However, it is not considered the most common risk factor when compared to maternal hypertension.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
The correct answer is choice c. Dry the newborn.
Choice A rationale:
Confirming identification and applying a bracelet is important for ensuring the newborn’s identity and preventing mix-ups, but it is not the immediate priority right after birth.
Choice B rationale:
Examining the newborn for birth defects is crucial for identifying any immediate health concerns, but it should be done after initial stabilization measures like drying and warming the newborn.
Choice C rationale:
Drying the newborn is the first action the nurse should take immediately after delivery. This helps to prevent heat loss and maintain the newborn’s body temperature, which is critical for their survival and well-being.
Choice D rationale:
Conducting a gestational age assessment is important for determining the newborn’s maturity and potential health risks, but it is not the immediate priority right after birth.
Correct Answer is C
Explanation
Choice C rationale:
This response is correct because black stools are a common side effect of taking iron supplements. Iron can cause the stool to appear black or
tarry due to the way it is broken down during digestion. It does not necessarily indicate a serious issue, especially if the client is not experiencing any abdominal pain or cramping. Educating the client about this expected side effect helps alleviate any concerns they might have about the change in stool colour.
Choice A rationale:
"Go to the emergency room and your provider will meet you there.”. This response is not appropriate in this situation. The client's report of black stools without abdominal pain or cramping is likely due to the iron supplements and does not warrant a visit to the emergency room. This response may cause unnecessary panic and anxiety for the client.
Choice B rationale:
"What else have you been eating?.”. This response is also not the best choice. While it's essential for healthcare providers to gather comprehensive information about a client's diet and lifestyle, in this case, the client's black stools can be directly attributed to the iron supplements. Focusing on other dietary factors might distract from addressing the client's concern about the side effect of iron supplementation.
Choice D rationale:
"Come to the office, and we will check things out.”. This response is not the most appropriate one either. A visit to the office might not be necessary solely based on the client's report of black stools without accompanying pain or cramping. This situation can be managed through education, and the client can be reassured that it is a typical side effect of iron supplements. An unnecessary visit to the office could inconvenience the client and waste both their time and the healthcare provider's time.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
