A nurse received a prescription to administer a medication NOW to a client. Which action should the nurse take?
Administer the medication within 90 minutes of the provider prescribing the medication.
Administer the medication at specific times until directed by the provider.
Administer the medication at every 4-hour intervals.
Administer the medication whenever the client reports specific manifestations, such as pain.
The Correct Answer is A
Choice A reason: Administering the medication within 90 minutes of the provider prescribing it aligns with the definition of a “NOW” order. A “NOW” order is intended to be given promptly but not as urgently as a STAT order, which requires immediate administration. This timeframe ensures that the medication is given in a timely manner to address the client’s needs without unnecessary delay.
Choice B reason: Administering the medication at specific times until directed by the provider is not appropriate for a “NOW” order. This approach is more suitable for routine or scheduled medications, where the timing is predetermined and consistent. A “NOW” order requires prompt action rather than adherence to a fixed schedule.
Choice C reason: Administering the medication at every 4-hour intervals is incorrect for a “NOW” order. This frequency is typical for PRN (as needed) medications or those requiring regular dosing intervals. A “NOW” order is a one-time directive that necessitates timely administration soon after the order is given.
Choice D reason: Administering the medication whenever the client reports specific manifestations, such as pain, is characteristic of PRN orders. PRN orders are given based on the client’s symptoms and needs at the time. A “NOW” order, however, is a one-time order that should be carried out promptly, regardless of the client’s immediate symptoms.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
Choice A Reason:
When calculating the fluid balance for a client undergoing continuous bladder irrigation (CBI), the irrigation solution must be deducted from the total urine output. This is because the irrigation fluid is not part of the client’s actual urine production but is an additional fluid introduced into the bladder to prevent or remove blood clots and ensure catheter patency. By deducting the irrigation solution from the total urine output, the nurse can accurately determine the client’s true urine output and fluid balance.
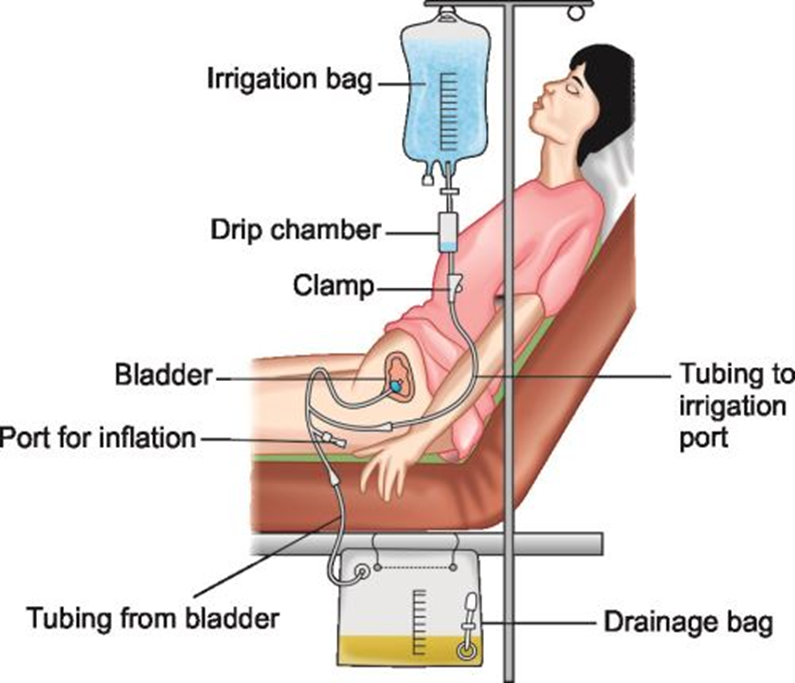
Choice B Reason:
Subtracting the irrigation solution from the intravenous flow sheet as output is incorrect. The intravenous flow sheet is used to document fluids administered intravenously, not those introduced into the bladder. Therefore, this choice does not apply to the management of continuous bladder irrigation.
Choice C Reason:
Documenting the intake hourly in the urine output column is also incorrect. The urine output column should reflect the actual urine produced by the client, not the irrigation solution. Including the irrigation solution in this column would lead to an inaccurate representation of the client’s urine output and fluid balance.
Choice D Reason:
Adding the irrigation solution to the oral intake column is incorrect as well. The oral intake column is designated for fluids consumed orally by the client. The irrigation solution is introduced directly into the bladder and should not be recorded as oral intake.
Correct Answer is A
Explanation
Choice A Reason:
Fiber is correct. Fiber is essential for maintaining healthy bowel elimination. It helps to add bulk to the stool and promotes regular bowel movements. There are two types of fiber: soluble and insoluble. Soluble fiber absorbs water and forms a gel-like substance, which helps soften the stool and make it easier to pass. Insoluble fiber adds bulk to the stool and helps it move through the digestive tract more quickly.
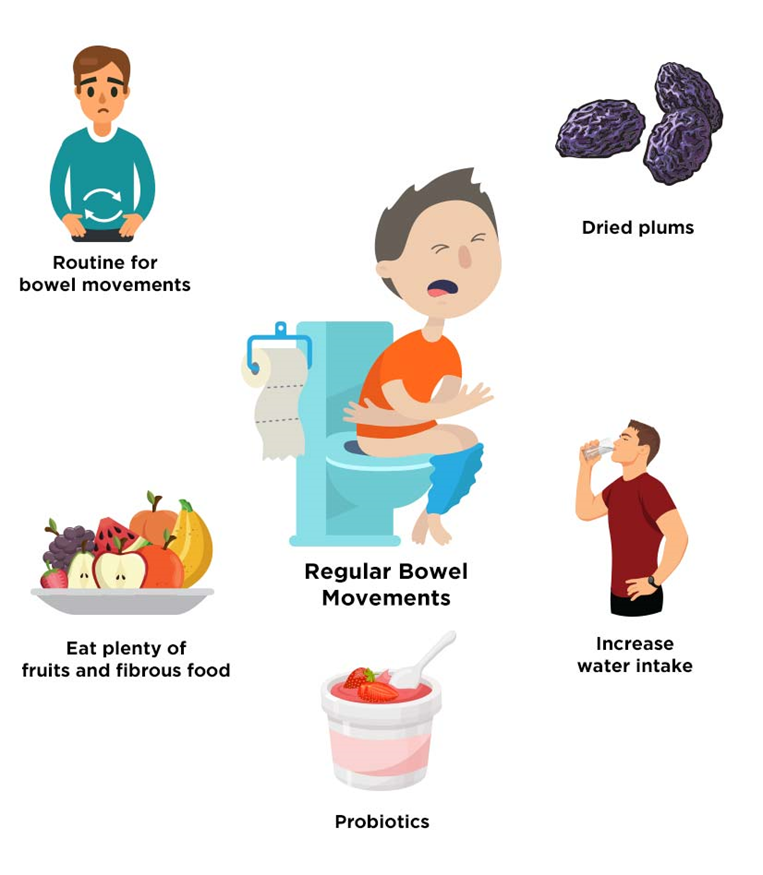
Choice B Reason:
Fat is incorrect. While fats are an important part of a balanced diet, they do not play a primary role in maintaining healthy bowel elimination. Fats are essential for energy and the absorption of fat-soluble vitamins, but they do not have the same effect on bowel movements as fiber.
Choice C Reason:
Protein is incorrect. Protein is crucial for building and repairing tissues, but it does not directly influence bowel elimination. A diet high in protein without adequate fiber can sometimes lead to constipation.
Choice D Reason:
Minerals are incorrect. Minerals are vital for various bodily functions, including bone health, fluid balance, and muscle function. However, they do not directly impact bowel elimination in the same way that fiber does.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
