A patient experiencing multisystem fluid volume deficit has tachycardia, pale, cool skin, and decreased urine output. The nurse realizes these findings are most likely a direct result of which process?
Effects of rapidly infused intravenous fluids.
The body's natural compensatory mechanisms.
Cardiac failure.
Pharmacological effects of a diuretic.
The Correct Answer is B
Choice A Reason: This is incorrect because effects of rapidly infused intravenous fluids are not the cause of the patient's findings, but a possible treatment. Rapidly infused intravenous fluids are used to restore fluid volume and prevent shock in patients with fluid volume deficit. Rapidly infused intravenous fluids can cause increased blood pressure, increased urine output, and decreased heart rate.
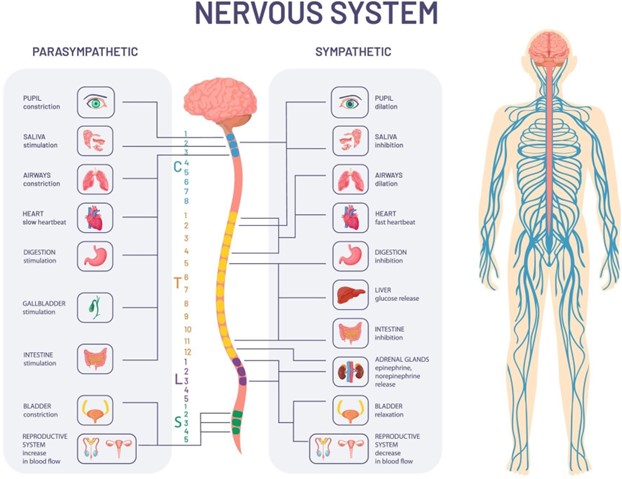
Choice B Reason: This is correct because the body's natural compensatory mechanisms are the cause of the patient's findings. The body tries to maintain homeostasis and perfusion in response to fluid volume deficit by activating the sympathetic nervous system, the renin-angiotensin-aldosterone system, and the antidiuretic hormone system. These mechanisms cause tachycardia, vasoconstriction, pale and cool skin, sodium and water retention, and decreased urine output.
Choice C Reason: This is incorrect because cardiac failure is not the cause of the patient's findings, but a possible complication. Cardiac failure occurs when the heart is unable to pump enough blood to meet the body's needs. Cardiac failure can result from prolonged fluid volume deficit, as the heart becomes overstressed and weakened by the increased workload and decreased perfusion. Cardiac failure can cause dyspnea, edema, fatigue, and cyanosis.
Choice D Reason: This is incorrect because pharmacological effects of a diuretic are not the cause of the patient's findings, but a possible cause of fluid volume deficit. A diuretic is a medication that increases urine output and excretion of sodium and water. A diuretic can cause fluid volume deficit if it is overdosed, misused, or taken with other medications that affect fluid balance. A diuretic can cause hypotension, dehydration, and electrolyte imbalances.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
Choice A: A patient with venous stasis ulcer is not at increased risk for metabolic alkalosis, because this condition does not affect the acid-base balance of the body. Venous stasis ulcer is a chronic wound that occurs due to impaired blood flow in the lower extremities.
Choice B: A patient on dialysis is not at increased risk for metabolic alkalosis, because dialysis helps to remove excess acids and bases from the blood. Dialysis is a treatment that filters and purifies the blood using a machine.
Choice C: A patient with bulimia is at increased risk for metabolic alkalosis, because this condition involves frequent vomiting that causes loss of gastric acid. Gastric acid is a source of hydrogen ions that lowers the pH of the blood. When gastric acid is lost, the blood becomes more alkaline.
Choice D: A patient with COPD is not at increased risk for metabolic alkalosis, but rather for respiratory acidosis. This is because COPD impairs the ability of the lungs to eliminate carbon dioxide, which is a source of carbonic acid that lowers the pH of the blood. When carbon dioxide accumulates, the blood becomes more acidic.
Correct Answer is ["A","B","D"]
Explanation
Choice A: Bicarbonate excess is a sign of metabolic alkalosis, because this condition occurs when the body has too much bicarbonate or loses too much acid. This can happen in patients who have excessive vomiting, gastric suctioning, diuretic therapy, or antacid intake.
Choice B: Lethargy is a sign of metabolic alkalosis, because this condition affects the central nervous system and causes decreased level of consciousness, confusion, and drowsiness. Lethargy can also result from hypoxemia, which is a condition that occurs when the blood oxygen level is too low. This can happen in patients with metabolic alkalosis who have respiratory compensation and hypoventilation.
Choice C: Kussmaul's respirations are not a sign of metabolic alkalosis, but rather of metabolic acidosis. This is a condition that occurs when the body produces too much acid or loses too much bicarbonate. This can happen in patients who have diabetic ketoacidosis, renal failure, or lactic acidosis. Kussmaul's respirations are deep, rapid, and labored breathing that help to eliminate excess carbon dioxide and acid from the blood.
Choice D: Circumoral paresthesia is a sign of metabolic alkalosis, because this condition causes hypocalcemia, which is a condition that occurs when the blood calcium level is too low. This can happen in patients with metabolic alkalosis who have increased binding of calcium to albumin due to alkaline pH. Circumoral paresthesia is a tingling sensation around the mouth that indicates neuromuscular irritability.
Choice E: Flushing is not a sign of metabolic alkalosis, but rather of hypercalcemia, which is a condition that occurs when the blood calcium level is too high. This can happen in patients who have hyperparathyroidism, malignancy, or excessive calcium intake. Flushing is a reddening of the skin that indicates vasodilation and increased blood flow.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
