A patient who is experiencing chest pain and shortness of breath is brought to the emergency department.
The nurse assesses a heart rate of 98 beats per minute, bilateral lung crackles, and an oxygen saturation of 90%. What will the nurse expect to administer initially to this patient?
Albuterol (Proventil)
Oxygen
Nitroglycerin
Aspirin
The Correct Answer is B
Choice A rationale:
Albuterol (Proventil) is a bronchodilator that is used to treat acute asthma attacks and chronic obstructive pulmonary disease (COPD). It works by relaxing the smooth muscles in the airways, which allows more air to flow into the lungs. While albuterol can be helpful in relieving shortness of breath, it is not the first-line treatment for a patient with chest pain and low oxygen saturation. This is because albuterol does not address the underlying cause of the chest pain, which is likely a lack of oxygen to the heart muscle.
Choice C rationale:
Nitroglycerin is a vasodilator that is used to treat angina (chest pain) and heart failure. It works by relaxing the blood vessels, which allows more blood to flow to the heart. Nitroglycerin can be helpful in relieving chest pain, but it is not the first-line treatment for a patient with low oxygen saturation. This is because nitroglycerin can actually worsen hypoxemia (low oxygen levels in the blood) by dilating blood vessels in the lungs.
Choice D rationale:
Aspirin is a blood thinner that is used to prevent and treat blood clots. It is often given to patients with chest pain who are suspected of having a heart attack. However, aspirin is not the first-line treatment for a patient with low oxygen saturation. This is because aspirin does not address the underlying cause of the low oxygen saturation, which is likely a problem with the lungs or heart.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
Choice A rationale:
Stevens-Johnson syndrome (SJS) is a rare, serious skin condition that is typically caused by an allergic reaction to medication. While amiodarone has been associated with a few cases of SJS, it is not considered a common long-term side effect.
Choice B rationale:
Ventricular tachycardia (VT) is a type of fast heart rhythm that originates in the ventricles of the heart. Amiodarone is actually used to treat VT, so it would be counterintuitive to list it as a long-term side effect.
Choice C rationale:
Pulmonary fibrosis is a condition characterized by scarring of the lung tissue. While amiodarone can cause pulmonary toxicity, which includes pulmonary fibrosis, this is a relatively rare side effect. Moreover, it's usually associated with high doses or
long-term use of the medication.
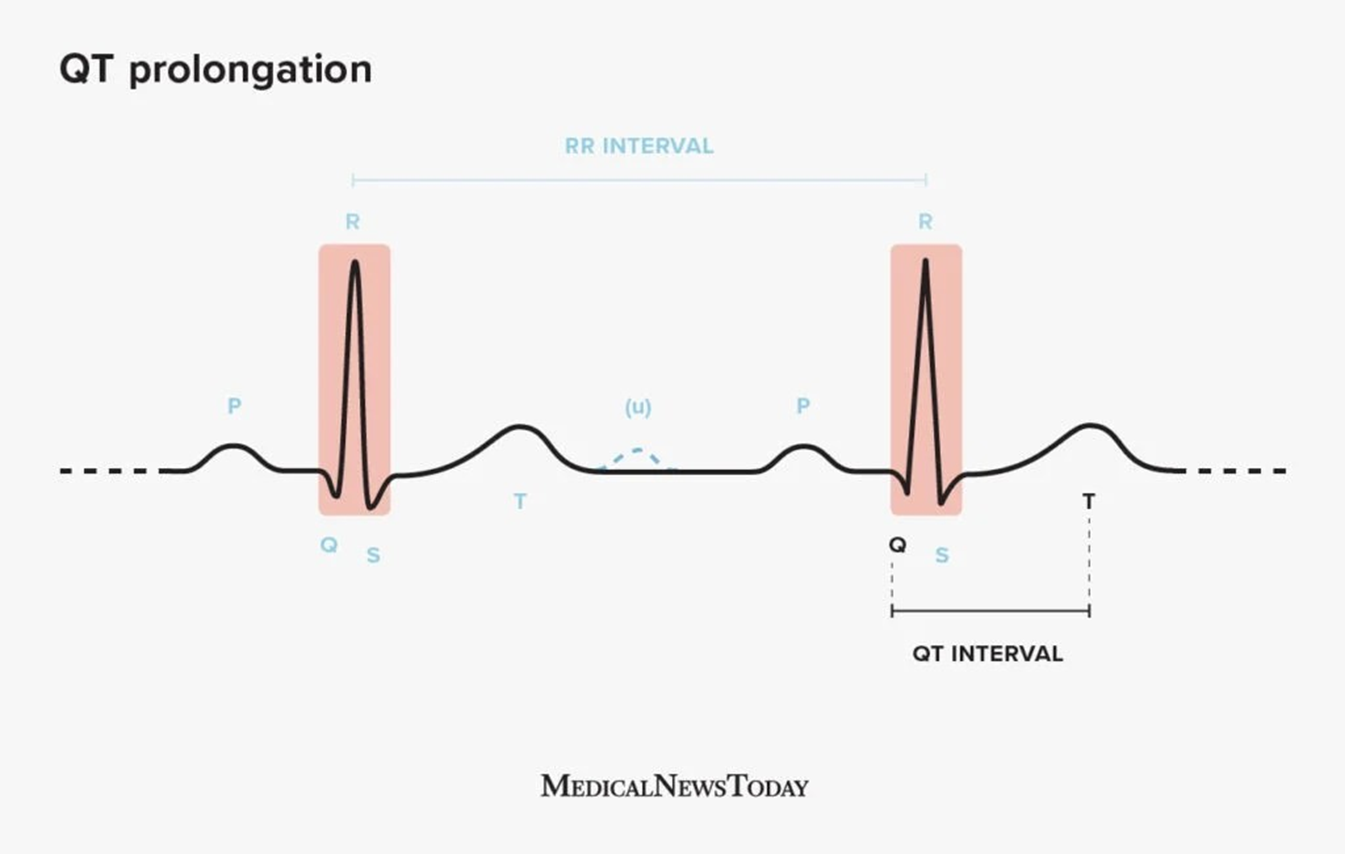
Choice D rationale:
QT prolongation is a condition in which the heart's electrical activity takes longer than normal to recharge between beats. This can lead to a potentially fatal arrhythmia called torsades de pointes. Amiodarone is known to prolong the QT interval, and this is considered one of its most significant long-term side effects. It's important to monitor patients on amiodarone for QT prolongation and to adjust the dose or discontinue the medication if necessary.
Correct Answer is B
Explanation
Choice A rationale:
Incorrect. Insulin pumps should be removed before bathing or swimming to prevent damage to the device. Water can enter the pump through the infusion set or through the battery compartment, causing it to malfunction. This can lead to inaccurate insulin delivery, which can result in hyperglycemia or hypoglycemia.
Additionally, the adhesive that holds the infusion set in place may not stick well to wet skin, which can increase the risk of the infusion set falling out.
It is important to note that some insulin pumps are now waterproof and can be worn while bathing or swimming. However, it is still important to check the manufacturer's instructions before doing so.
Choice B rationale:
Correct. Even though insulin pumps deliver insulin continuously, people who use them still need to monitor their blood glucose levels regularly. This is because many factors can affect blood glucose levels, such as food intake, exercise, stress, and illness.
Monitoring blood glucose levels allows people to adjust their insulin doses as needed to keep their blood glucose levels within a target range.
Recommended frequency of blood glucose monitoring:
Before meals and snacks Two hours after meals At bedtime
Before and after exercise During times of illness or stress
Whenever they feel symptoms of hypoglycemia or hyperglycemia
Choice C rationale:
Incorrect. People who use insulin pumps still need to count carbohydrates. This is because the amount of insulin that is needed to cover a meal depends on the amount of carbohydrates in the meal.
The insulin pump can be programmed to deliver different amounts of insulin for different meals, snacks, and corrections based on carbohydrate intake. This allows for more precise insulin dosing and better blood glucose control.
Choice D rationale:
Incorrect. Insulin pumps are not designed to help people lose weight. They are designed to help people manage their blood glucose levels.
While some people may lose weight when they start using an insulin pump, this is usually due to improved blood glucose control rather than the pump itself.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
