After initiating a steroid nebulizer treatment for a client with asthma in respiratory distress, which intervention is most important for the nurse to implement?
Monitor pulse oximetry every 2 hours.
Teach proper use of a rescue inhaler.
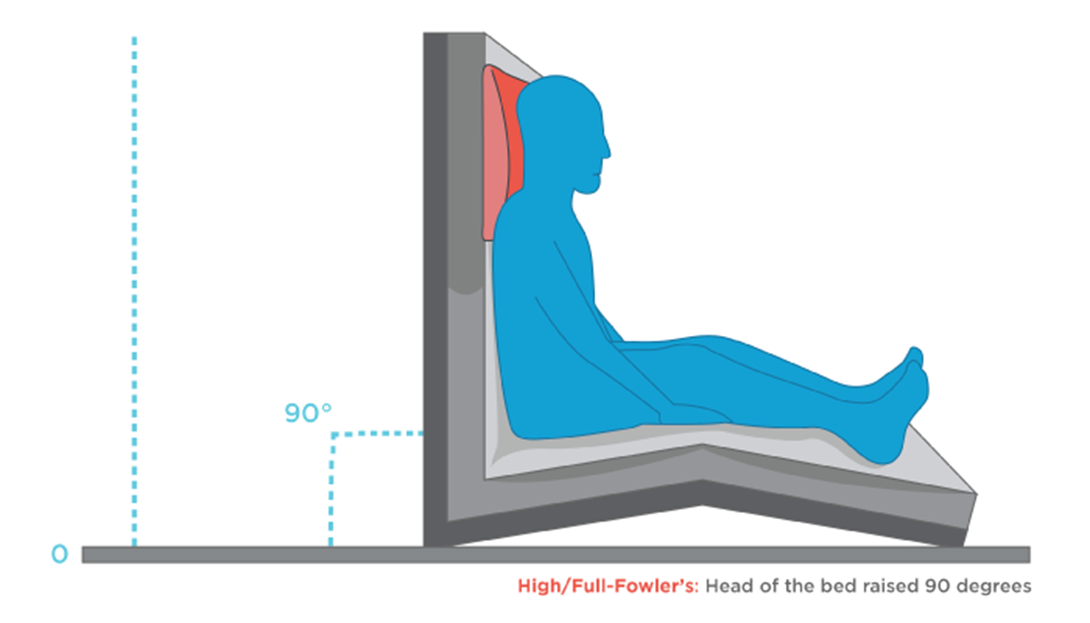
Elevate the head of bed to 90 degrees.
Determine exposure to asthmatic triggers.
The Correct Answer is C
Choice A reason: This is incorrect because monitoring pulse oximetry every 2 hours is not a sufficient or timely intervention for the nurse to implement. Pulse oximetry is a noninvasive method of measuring the oxygen saturation of hemoglobin in the blood. Normal oxygen saturation is 95% to 100%, while hypoxemia is less than 90%. However, pulse oximetry may not reflect the severity of respiratory distress or the effectiveness of nebulizer treatment in a client with asthma. Moreover, monitoring pulse oximetry every 2 hours is too infrequent for a client who is in acute respiratory distress and needs more frequent assessment and intervention.
Choice B reason: This is incorrect because teaching proper use of a rescue inhaler is not a priority or relevant intervention for the nurse to implement. A rescue inhaler is a type of short-acting bronchodilator that can be used to relieve acute asthma symptoms by relaxing the smooth muscles of the airways and improving airflow. However, teaching proper use of a rescue inhaler is not an urgent action for a client who is already receiving nebulizer treatment, which delivers a higher dose of medication directly to the lungs. Moreover, teaching proper use of a rescue inhaler is not appropriate for a client who is in respiratory distress and may not be able to focus or retain information.
Choice C reason: This is correct because elevating the head of bed to 90 degrees is the most important intervention for the nurse to implement. Elevating the head of bed to 90 degrees can help improve breathing and oxygenation by reducing pressure on the diaphragm and chest wall, increasing lung expansion and ventilation, and facilitating expectoration of mucus. This can enhance the effects of nebulizer treatment and reduce respiratory distress in a client with asthma.
Choice D reason: This is incorrect because determining exposure to asthmatic triggers is not an immediate or helpful intervention for the nurse to implement. Asthmatic triggers are substances or factors that can cause or worsen asthma symptoms by inducing inflammation or constriction of the airways. Examples of asthmatic triggers include allergens, irritants, infections, exercise, stress, or weather changes. However, determining exposure to asthmatic triggers is not a priority action for a client who is in respiratory distress and needs more urgent interventions to improve breathing and oxygenation. Moreover, determining exposure to asthmatic triggers may not change the management or outcome of an acute asthma attack that has already occurred.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
Choice A: A headache rated at 0 on 0 to 10 scale is not a specific indicator of the effectiveness of an antihistamine. A headache may be caused by other factors, such as dehydration, stress, or sinus congestion.
Choice B: Oxygen saturation level of 99% is a normal finding and does not reflect the effect of an antihistamine. Oxygen saturation measures the amount of oxygen in the blood and can be affected by respiratory conditions, altitude, or smoking.
Choice C: Ambulating easily without vertigo is a sign that the antihistamine is effective. Vertigo is a common symptom of Ménière's disease, which is a disorder of the inner ear that causes episodes of spinning sensation, hearing loss, and tinnitus. Antihistamines can help reduce the fluid buildup in the inner ear and relieve vertigo.
Choice D: Blood pressure of 120/80 mm Hg is a normal finding and does not indicate the effect of an antihistamine. Blood pressure measures the force of blood against the walls of the arteries and can be influenced by factors such as heart rate, cardiac output, blood volume, and vascular resistance.

Correct Answer is C
Explanation
Choice A reason: This is incorrect because sleeping with the head ofthe bed flat can worsen OSA by allowing gravity to pull down on the soft tissues ofthe throat and obstructing airflow.
Choice B reason: This is incorrect because taking sedatives prior to sleep can also worsen OSA by relaxing the muscles ofthe upper airway and increasing airway collapse.
Choice C reason: This is correct because beginning a weight loss program can help reduce OSA by decreasing fat deposits around the neck and chest that can compress and narrow the airway.
Choice D reason: This is incorrect because drinking 1to 2 glasses of wine at bedtime can have similar effects as sedatives, such as relaxing the muscles ofthe upper airway and impairing the respiratory drive.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
