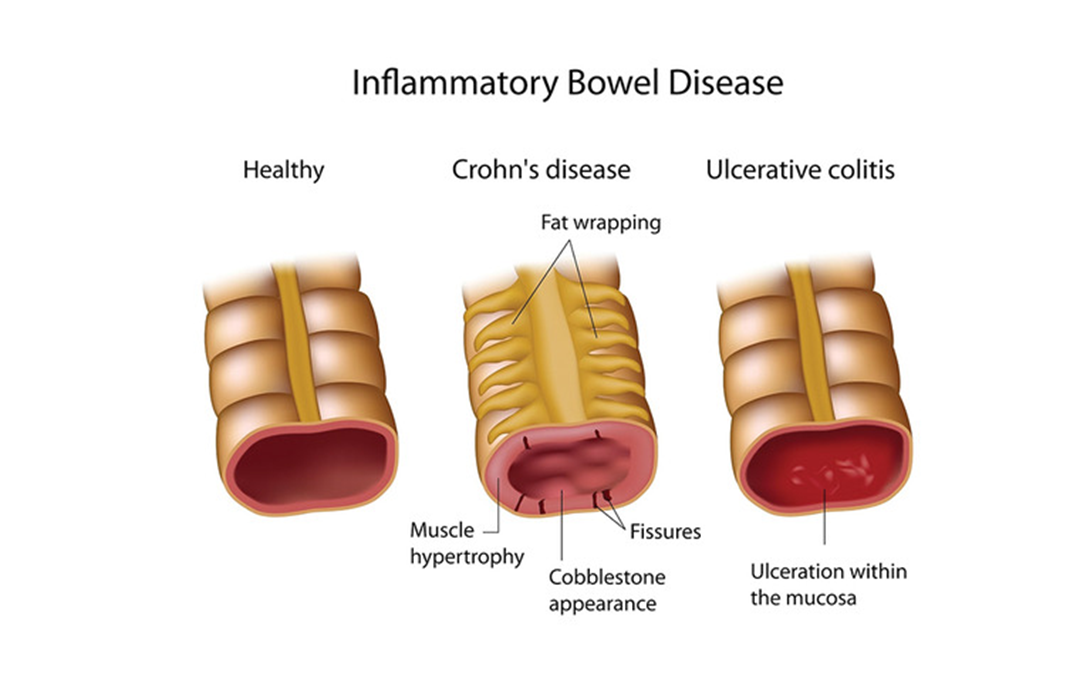
A client is hospitalized with an inflammatory bowel disease (IBD) exacerbation and is being treated with a corticosteroid. The client develops a rigid abdomen with rebound tenderness. Which action should the nurse take?
Measure capillary glucose level.
Encourage ambulation in the room.
Monitor for bloody diarrheal stools.
Obtain vital sign measurements.
The Correct Answer is D
Choice A reason: Measuring capillary glucose level is not a priority action for a client with a rigid abdomen and rebound tenderness. These signs indicate peritonitis, which is a serious complication of IBD that requires immediate attention. Corticosteroids can increase blood glucose levels, but this is not an urgent concern in this situation.
Choice B reason: Encouraging ambulation in the room is not appropriate for a client with a rigid abdomen and rebound tenderness. These signs indicate peritonitis, which is a serious complication of IBD that requires immediate attention. Ambulation can worsen the pain and inflammation, and increase the risk of bowel perforation.
Choice C reason: Monitoring for bloody diarrheal stools is important for a client with IBD, but not a priority action for a client with a rigid abdomen and rebound tenderness. These signs indicate peritonitis, which is a serious complication of IBD that requires immediate attention. Bloody stools can be a sign of ulceration or bleeding in the bowel, but they are not specific to peritonitis.
Choice D reason: Obtaining vital sign measurements is the priority action for a client with a rigid abdomen and rebound tenderness. These signs indicate peritonitis, which is a serious complication of IBD that requires immediate attention. Vital signs can reveal signs of infection, inflammation, shock, and organ failure, which can guide the appropriate interventions and treatments.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
Choice A reason: Returning for periodic liver function studies is an important instruction for a client with gouty arthritis who is taking colchicine and indomethacin. These medications can cause liver toxicity, which can manifest as jaundice, abdominal pain, nausea, vomiting, and dark urine. The nurse should advise the client to monitor for these signs and symptoms, and to have regular blood tests to check the liver enzymes and function.
Choice B reason: Massaging joints to relax muscles and decrease pain is not a recommended instruction for a client with gouty arthritis who has acute inflammation of the right ankle and great toe. Massage can increase the blood flow and pressure to the affected joints, which can worsen the pain and swelling. The nurse should advise the client to avoid touching or moving the inflamed joints, and to apply ice packs or cold compresses to reduce the inflammation.
Choice C reason: Limiting use of mobility equipment to avoid muscle atrophy is not a necessary instruction for a client with gouty arthritis who has acute inflammation of the right ankle and great toe. Mobility equipment such as crutches, walkers, or canes can help the client to ambulate safely and comfortably, and to prevent further injury or damage to the affected joints. The nurse should encourage the client to use mobility equipment as needed, and to perform gentle range of motion exercises when the inflammation subsides.
Choice D reason: Substituting natural fruit juices for carbonated drinks is not a helpful instruction for a client with gouty arthritis who is taking colchicine and indomethacin. Fruit juices can contain high amounts of fructose, which can increase the uric acid levels in the blood and trigger gout attacks. Carbonated drinks are not a major risk factor for gout, unless they contain high-fructose corn syrup or alcohol. The nurse should advise the client to drink plenty of water, and to avoid foods and beverages that are high in purines, such as organ meats, seafood, beer, and wine.
Correct Answer is []
Explanation
Focused assesment area : Neurological
The correct answer is B. Speaks in short sentences.
Choice A: Drinks with repetitive cough. This is an incorrect answer because it indicates that the patient has difficulty swallowing, which is a common complication of ischemic stroke. Swallowing problems can lead to aspiration pneumonia, dehydration, and malnutrition. Therefore, this finding does not indicate effective early intervention for ischemic stroke¹.
Choice B: Speaks in short sentences. This is a correct answer because it indicates that the patient's speech has improved from being garbled to being intelligible. Speech impairment is a common symptom of ischemic stroke, especially when the left hemisphere of the brain is affected. Early intervention with thrombolytic therapy or mechanical thrombectomy can restore blood flow to the affected brain tissue and reduce the extent of damage². Therefore, this finding indicates effective early intervention for ischemic stroke.
Choice C: Decorticate posturing. This is an incorrect answer because it indicates that the patient has severe brain damage and is in a state of coma. Decorticate posturing is a type of abnormal posture that occurs when the upper limbs flex and the lower limbs extend in response to pain or stimulation. It indicates damage to the cerebral hemispheres or the internal capsule³. Therefore, this finding does not indicate effective early intervention for ischemic stroke.
Focused assesment area : Muscoskeletal
The correct answer is B. Ambulates with a walker.
Choice A: Flaccidity of left arm. This is an incorrect answer because it indicates that the patient has weakness or paralysis of the left arm, which is a common symptom of ischemic stroke. Flaccidity is the absence of muscle tone or resistance to passive movement. It indicates damage to the motor cortex or the corticospinal tract. Therefore, this finding does not indicate effective early intervention for ischemic stroke.
Choice B: Ambulates with a walker. This is a correct answer because it indicates that the patient has regained some mobility and independence after the ischemic stroke. Ambulation is the ability to walk or move from one place to another. Early intervention with physical therapy and rehabilitation can help improve the patient's functional recovery and prevent complications such as deep vein thrombosis, pressure ulcers, and contractures. Therefore, this finding indicates effective early intervention for ischemic stroke.
Choice C: Passive range of motion on left leg. This is an incorrect answer because it indicates that the patient has limited or no voluntary movement of the left leg, which is another common symptom of ischemic stroke. Passive range of motion is the movement of a joint or limb by an external force, such as a therapist or a caregiver. It indicates damage to the motor cortex or the corticospinal tract. Therefore, this finding does not indicate effective early intervention for ischemic stroke.
Focused assesment area : Psychosocial
The correct answer is B. Tearful sharing of stories.
Choice A: Fits of laughter. This is an incorrect answer because it indicates that the patient has inappropriate emotional responses, which is a common complication of ischemic stroke. Inappropriate emotional responses are sudden and uncontrollable episodes of laughing or crying that are out of context or disproportionate to the situation. They indicate damage to the brain regions that regulate emotions, such as the frontal lobe, the thalamus, or the brainstem. Therefore, this finding does not indicate effective early intervention for ischemic stroke.
Choice B: Tearful sharing of stories. This is a correct answer because it indicates that the patient has improved social and emotional functioning after the ischemic stroke. Tearful sharing of stories is a normal and healthy way of expressing emotions and coping with stress. It also shows that the patient has preserved memory and language skills, which are often impaired by ischemic stroke. Early intervention with psychological support and counseling can help the patient deal with the emotional impact of stroke and improve their quality of life. Therefore, this finding indicates effective early intervention for ischemic stroke.
Choice C: Angry outburst. This is an incorrect answer because it indicates that the patient has mood disturbances, which is another common complication of ischemic stroke. Mood disturbances are changes in the patient's emotional state, such as depression, anxiety, irritability, or aggression. They indicate damage to the brain regions that regulate mood, such as the frontal lobe, the amygdala, or the hippocampus. Therefore, this finding does not indicate effective early intervention for ischemic stroke.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
