In caring for a client following a head injury, the nurse plans to assess for rhinorrhea so that a sample can be tested for the presence of cerebrospinal fluid (CSF). At which location should the nurse observe for this finding?
(Click the chosen location. To change, click on the new location.)
The Correct Answer is "{\"xRanges\":[389.5,439.5],\"yRanges\":[222,272]}"
Site- the nose
Rationale
Rhinorrhea refers specifically to cerebrospinal fluid (CSF) rhinorrhea. This occurs when there is a leakage of CSF from the nose due to a fracture or injury to the skull base or surrounding structures, such as the cribriform plate.
CSF is a clear fluid that surrounds and cushions the brain and spinal cord. When there is a fracture or disruption in the skull base, CSF can leak out through the nasal passages. This condition is concerning because it can increase the risk of infection, such as meningitis, due to the direct communication between the central nervous system and the external environment through the nasal cavity.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is {"A":{"answers":"A"},"B":{"answers":"C"},"C":{"answers":"B"},"D":{"answers":"B"}}
Explanation
Client Statement: A. The client seems unemotional when talking about needing to rebuild her house.
Suppression fits here because the client appears detached or unemotional when discussing the significant emotional task of rebuilding her house after it collapsed. This suggests a deliberate effort to suppress or minimize the emotional impact of the situation.
Client Statement: C. The client discusses moving to Hawaii instead of returning to rebuild her house.
The client's discussion of moving to Hawaii instead of facing the reality of rebuilding her house reflects a form of fantasy. It suggests a retreat into an idealized scenario (moving to a distant, idyllic location) to avoid dealing directly with the trauma and stress associated with rebuilding her home.
Client Statement: B. The client says that she sometimes forgets why she is in the hospital.
Isolation can be inferred here because the client's statement about forgetting why she is in the hospital may indicate a psychological distancing or detachment from the traumatic events that led her there. It suggests a coping mechanism where she separates her emotional distress (related to the house collapse) from the practical reality of being hospitalized and receiving treatment.
Client Statement: D. The client is frightened that the hospital will burn down.
This statement fits into the defense mechanisms of fantasy. The client encounters thoughts of the hospital burning and her house burns down.
Correct Answer is C
Explanation
Rationale
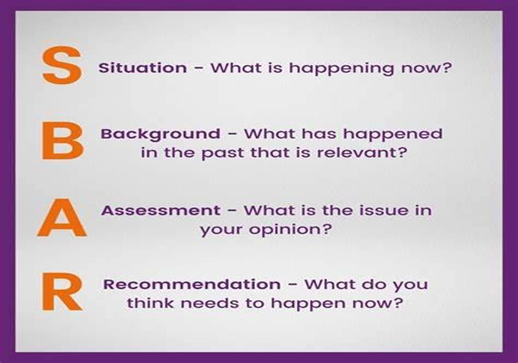
A. While it is important background information, it is not directly relevant to the acute change in the client's condition (increasing confusion and agitation). Therefore, this should not be provided first in the SBAR communication.
B. Knowing the client's current medications is important for understanding any potential causes or exacerbating factors related to the sudden onset of confusion and agitation. However, this is also background information and does not immediately address the acute change in the client's condition.
C. This is the most critical piece of information to provide first in the SBAR communication. Sudden onset of increasing confusion and agitation can indicate various urgent issues such as delirium, infection, metabolic disturbances, or neurological complications. This requires immediate attention and intervention from the healthcare provider.
D. While knowing the client's healthcare power of attorney is important for ensuring appropriate decision-making if needed, it is not urgent information in the context of reporting a sudden change in the client's condition. This can be discussed later in the SBAR communication or as part of the background information if relevant to the client's care.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
