In evaluating the effectiveness of a postoperative client's intermittent pneumatic compression devices, which assessment is most important for the nurse to complete?
Palpate all peripheral pulse points for volume and strength.
Monitor the amount of drainage from the client's incision.
Observe both lower extremities for redness and swelling.
Evaluate the client's ability to use an incentive spirometer.
The Correct Answer is C
The correct answer is choice C. Observe both lower extremities for redness and swelling.
Choice A rationale:
Palpating all peripheral pulse points for volume and strength is important for assessing circulation, but it does not directly evaluate the effectiveness of intermittent pneumatic compression (IPC) devices. IPC devices are primarily used to prevent deep vein thrombosis (DVT) and improve venous return, so monitoring for signs of DVT is more relevant.
Choice B rationale:
Monitoring the amount of drainage from the client’s incision is crucial for assessing wound healing and detecting potential infections, but it is not related to the effectiveness of IPC devices.
Choice C rationale:
Observing both lower extremities for redness and swelling is the most important assessment for evaluating the effectiveness of IPC devices. Redness and swelling can be signs of DVT, which IPC devices are designed to prevent. Therefore, this assessment directly measures whether the devices are functioning as intended.
Choice D rationale:
Evaluating the client’s ability to use an incentive spirometer is important for preventing postoperative pulmonary complications, but it does not assess the effectiveness of IPC devices.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
Tertiary prevention programs focus on minimizing the impact of an existing disease or condition and preventing further complications or disability. In the context of cardiovascular disease, one of the goals of tertiary prevention is to provide prompt rehabilitation for clients who have incurred disease complications.
By ensuring that clients who experience complications promptly receive rehabilitation services, the program is effectively addressing the needs of these clients and providing appropriate interventions to minimize the long-term impact of the disease. This outcome indicates that the program is successful in providing the necessary care and support to clients with cardiovascular disease.
Client relapse rate of 30% in a 5-year community-wide anti-smoking campaign focuses on primary prevention rather than tertiary prevention.
At-risk clients receiving an increased number of routine health screenings may be an indicator of improved secondary prevention efforts, but it does not specifically measure the effectiveness of the tertiary prevention program for clients with cardiovascular disease.
Clients reporting new confidence in making healthy food choices is a positive outcome but does not directly reflect the effectiveness of the tertiary prevention program for cardiovascular disease.
Correct Answer is A
Explanation
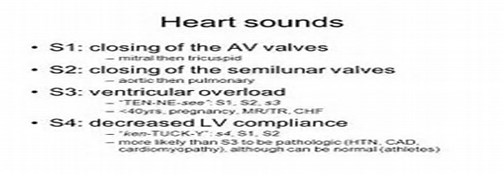
An S3 heart sound can be a normal finding during pregnancy due to increased blood volume and changes in cardiac output. It is known as a physiological S3 and is considered a benign finding in the absence of other concerning symptoms or signs.
In this case, there is no immediate need for intervention or concern regarding the S3 heart sound. It is not necessary to prepare the client for an echocardiogram or limit the client's fluids based solely on the presence of an S3 heart sound in the absence of other significant symptoms or complications.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
