A glucagon emergency kit is prescribed for a client with type 1 diabetes mellitus. When should the nurse instruct the client and family that glucagon needs to be administered?
If severe hypoglycemia occurs.
Before meals to prevent hyperglycemia.
When unable to eat during sick days.
At the onset of signs of diabetic ketoacidosis.
The Correct Answer is A
Choice A Reason:
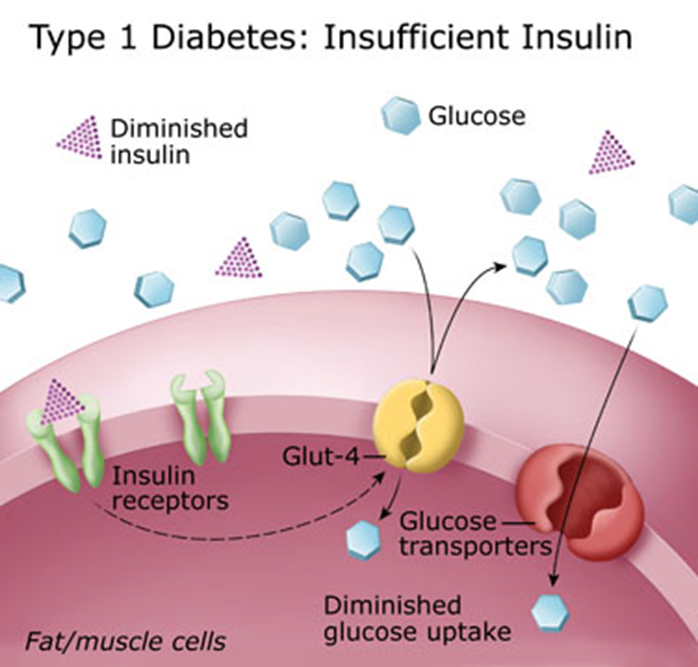
Glucagon is a hormone used to treat severe hypoglycemia (low blood sugar) in individuals with diabetes. Severe hypoglycemia can be life-threatening and requires immediate treatment to raise blood sugar levels. Glucagon works by stimulating the liver to release stored glucose into the bloodstream. It is crucial for clients and their families to recognize the signs of severe hypoglycemia, such as confusion, unconsciousness, or seizures, and to administer glucagon promptly.
Choice B Reason:
Administering glucagon before meals to prevent hyperglycemia is incorrect. Glucagon is not used to prevent high blood sugar levels; it is specifically used to treat low blood sugar levels. Preventing hyperglycemia typically involves insulin administration and dietary management, not glucagon.
Choice C Reason:
While managing blood sugar levels during sick days is important, glucagon is not used for this purpose. Clients are usually advised to monitor their blood sugar levels more frequently and adjust their insulin doses as needed during illness. Glucagon is reserved for emergency situations involving severe hypoglycemia.
Choice D Reason:
Glucagon is not used to treat diabetic ketoacidosis (DKA). DKA is a serious complication of diabetes that requires immediate medical attention and is treated with insulin, fluids, and electrolytes. Administering glucagon would not address the underlying issues of DKA and could potentially worsen the condition.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
Choice A Reason:
Avoiding taking the medication on an empty stomach is important to reduce gastrointestinal upset. Lithium can cause stomach irritation, and taking it with food can help mitigate this side effect. However, while this is good advice, it is not the most critical instruction to emphasize.
Choice B Reason:
Reporting fluctuations in weight to the healthcare provider is essential because significant weight changes can indicate potential side effects or complications from lithium therapy. Weight gain or loss can be a sign of thyroid dysfunction or other metabolic issues. While important, it is not the primary instruction to emphasize.
Choice C Reason:
Maintaining a fluid intake of 1500 to 2000 mL per day is crucial for clients taking lithium. Lithium levels in the blood can be affected by fluid balance, and dehydration can lead to lithium toxicity. Ensuring adequate hydration helps maintain stable lithium levels and reduces the risk of toxicity. This is the most critical instruction to emphasize to ensure the client’s safety and effective management of their condition.
Choice D Reason:
Keeping medication fliers for frequent review and reference is helpful for understanding the medication and its potential side effects. However, it is not the most critical instruction. The primary focus should be on maintaining proper hydration to prevent lithium toxicity.
Correct Answer is C
Explanation
Choice A reason:
Counting the apical and radial pulses simultaneously can help detect pulse deficits, which may indicate cardiac issues. However, this is not the most critical assessment for a client receiving hydromorphone.
Choice B reason:
Observing for edema around the ankles is important for assessing fluid retention and potential heart failure. While relevant, it is not the primary concern for a client on hydromorphone.
Choice C reason:
Auscultating the client’s bowel sounds is crucial because hydromorphone, like other opioids, can cause constipation and potentially lead to paralytic ileus, a serious condition where the intestines stop moving food through. Monitoring bowel sounds helps detect early signs of this complication.
Choice D reason:
Measuring the client’s capillary glucose level is important for diabetic patients or those at risk of hyperglycemia. However, it is not directly related to the administration of hydromorphone.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
