Order: Diphenhydramine 25mg Q4H
Available: Diphenhydramine 12.5mg/5mL
How much will you administer?
2 mL
10 mL
25mL
12.5 mL
The Correct Answer is B
First, we need to find out how many milligrams (mg) are in 1 milliliter (mL) of the available diphenhydramine solution:
12.5 mg/5 mL
To find out how many milligrams are in 1 mL, we divide the total milligrams by the total milliliters:
12.5 mg ÷ 5 mL = 2.5 mg/mL
Now that we know the concentration of diphenhydramine is 2.5 mg/mL, we can calculate the dose needed for the order of 25 mg:
25 mg ÷ 2.5 mg/mL = 10 mL
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
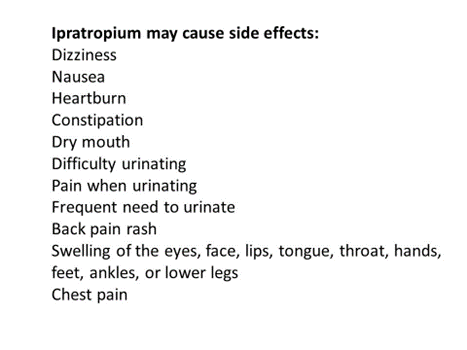
A. Dry mouth
Dry mouth is a common adverse effect of ipratropium (Atrovent) due to its anticholinergic properties. Anticholinergic medications can inhibit saliva production, leading to a sensation of dryness in the mouth. While uncomfortable, dry mouth tends to improve over time as the body adjusts to the medication. Patients can manage dry mouth by increasing fluid intake and practicing good oral hygiene.
B. Anxiety
Anxiety is not a common adverse effect of ipratropium (Atrovent). While some individuals may experience anxiety as a side effect of certain medications, it is not typically associated with ipratropium. If a patient experiences anxiety while taking ipratropium, it is essential to assess whether it may be related to other factors or medications and to consult a healthcare provider for appropriate management.
C. Tachycardia
Tachycardia (rapid heart rate) is not a common adverse effect of ipratropium (Atrovent). While ipratropium is an anticholinergic medication that can affect heart rate in some individuals, tachycardia is not typically reported as a common side effect. However, patients should be monitored for changes in heart rate and other cardiovascular effects while taking ipratropium, especially if they have pre-existing cardiac conditions.
D. Urine retention
Urinary retention is a potential adverse effect of ipratropium (Atrovent) due to its anticholinergic properties. Anticholinergic medications can relax the smooth muscle of the bladder, leading to difficulty emptying the bladder completely. However, urinary retention is less common with ipratropium compared to other anticholinergic medications, such as those used to treat overactive bladder. Patients experiencing urinary retention while taking ipratropium should consult their healthcare provider for further evaluation and management.
Correct Answer is C
Explanation
A. Saving the sputum specimen in a clean container.
While it is important to collect the sputum specimen in a clean, sterile container, simply saving the specimen in a clean container is not sufficient. The nurse needs to actively collect the sputum specimen from the client using proper technique to ensure that it is not contaminated and is suitable for laboratory analysis.
B. Collecting the sputum specimen after a meal.
Collecting a sputum specimen after a meal is not recommended, as it can increase the likelihood of contamination with food particles. It's preferable to collect the specimen before meals or at least 1-2 hours after eating to minimize the risk of contamination and ensure the integrity of the specimen.
C. Rinse the client's mouth before collecting the specimen.
When obtaining a sputum specimen from a client, it's important for the nurse to plan to rinse the client's mouth before collecting the specimen. Rinsing the mouth with water helps to clear any food particles or debris from the oral cavity, ensuring that the sputum sample collected is not contaminated with saliva or food particles. This improves the quality and accuracy of the specimen for laboratory analysis.
D. Obtaining the specimen from the client in the evening.
The timing of specimen collection is not necessarily restricted to the evening. The timing may vary depending on the client's condition and the healthcare provider's orders. It's important to follow the healthcare provider's instructions regarding the timing of specimen collection, which may be based on factors such as the client's symptoms and the diagnostic requirements.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
