The nurse is providing care to a client having surgery to repair a retinal detachment to the left eye. Which intervention should the nurse implement during the postoperative period?
Obtain vital signs every 2 hours during hospitalization.
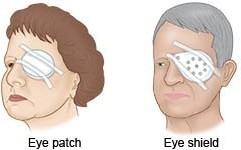
Provide an eye shield to be worn while sleeping.
Teach a family member to administer eye drops.
Encourage deep breathing and coughing exercises.
The Correct Answer is B
After retinal detachment surgery, it is crucial to protect the eye and the surgical repair site from accidental trauma or pressure. Providing an eye shield helps to shield the eye during sleep when the client may not have conscious control over their movements.
This can help prevent inadvertent rubbing or bumping of the eye, which could potentially disrupt the surgical repair and hinder the healing process.
Obtaining vital signs every 2 hours during hospitalization is a routine nursing intervention for postoperative care in general but is not specific to retinal detachment surgery. The frequency of vital sign monitoring may vary depending on the client's overall condition and the healthcare provider's orders.
Teaching a family member to administer eye drops may be necessary for the client's ongoing care, but it is not specifically related to the immediate postoperative period. Eye drop administration instructions can be provided as part of the client's discharge teaching.
Encouraging deep breathing and coughing exercises is a general postoperative intervention that promotes respiratory function and helps prevent complications such as pneumonia. While important for overall postoperative care, it is not specific to retinal detachment surgery.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
A) Incorrect- This is true; the diaphragm should be inserted before sexual activity. However, the main concern in this scenario is the need for refitting after childbirth.
B) Incorrect- This statement is not accurate. While the diaphragm is a form of contraception, it is not considered one of the most effective methods. Long-acting reversible contraceptives
(LARCs) like intrauterine devices (IUDs) and hormonal implants are among the most effective methods.
C) Incorrect- Vaseline lubricant can be used when inserting the diaphragm: Vaseline and other oil-based lubricants can weaken the latex or cause damage to the diaphragm. Water-based lubricants are recommended for use with diaphragms.
D) Correct- The diaphragm is a barrier contraceptive device that is inserted into the vagina before sexual intercourse to prevent pregnancy. However, its effectiveness can be compromised by changes in the anatomy of the vaginal canal, cervix, and pelvic structures, such as those that occur after childbirth. After vaginal childbirth, the pelvic structures may undergo changes, including stretching and possible loss of tone. These changes can affect the fit and position of the diaphragm, leading to decreased contraceptive efficacy. Therefore, it's important for women who have given birth to have their diaphragm refitted by a healthcare provider before resuming its use.

Correct Answer is D
Explanation
NPO status is crucial before a surgical procedure, especially when anesthesia will be administered. It helps prevent complications related to aspiration of gastric contents during the procedure. Failure to adhere to the NPO status can lead to serious respiratory problems, such as aspiration pneumonia.
It is important for the nurse to confirm the NPO status with the client to ensure that they have followed the appropriate fasting guidelines. This should be done to ensure the client's safety during the surgery.
While determining when the client last had pain medication, offering assistance to the restroom, and reviewing postoperative instructions are important aspects of preoperative care, confirming NPO status is the most critical nursing action in this particular scenario.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
