The practical nurse (PN) is assessing an older client with left-sided heart failure (HF). What intervention is most important for the PN to implement?
Inspect for sacral edema.
Measure urinary output.
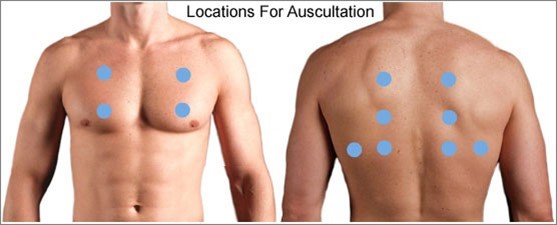
Auscultate all lung fields.
Check mental acuity.
The Correct Answer is C
When assessing an older client with left-sided heart failure (HF), the most important intervention for the practical nurse (PN) to implement is to auscultate all lung fields. Left-sided heart failure is characterized by the inability of the left ventricle to effectively pump blood, leading to fluid accumulation in the lungs. Auscultating all lung fields allows the PN to assess for the presence of abnormal lung sounds such as crackles, indicating pulmonary congestion.
Let's evaluate the other options:
a) Inspect for sacral edema.
Sacral edema is commonly associated with right-sided heart failure, not left-sided heart failure. While it is important to assess for edema in clients with heart failure, inspecting for sacral edema may not be the most immediate and crucial intervention in this specific case.
b) Measure urinary output.
Measuring urinary output is a valuable assessment in many clinical situations, but it may not be the most vital intervention in the context of left-sided heart failure. Monitoring urinary output is more relevant in assessing kidney function and fluid balance rather than directly assessing the severity of left-sided heart failure.
d) Check mental acuity.
Checking mental acuity is important in assessing the overall condition of the client, but it is not the most crucial intervention specifically related to left-sided heart failure. Mental status evaluation is more useful in identifying signs of altered mental status or potential complications, rather than directly assessing the impact of left-sided heart failure.
In summary, when assessing an older client with left-sided heart failure, the most important intervention for the practical nurse (PN) to implement is to auscultate all lung fields. This allows for the detection of abnormal lung sounds associated with pulmonary congestion, a hallmark sign of left-sided heart failure.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
When a preoperative client expresses fear and uncertainty about undergoing surgery, the priority action for the practical nurse (PN) is to notify the charge nurse of the client's concerns. This is important because the charge nurse can coordinate appropriate interventions and support for the client, ensuring their emotional well-being and addressing their fears.
Let's evaluate the other options:
a) Encourage the client to continue with the scheduled surgery.
While it is important to provide support and reassurance to the client, simply encouraging them to continue with the scheduled surgery may not adequately address their specific concerns and fears. The charge nurse and the healthcare team should be involved to provide the necessary support and information to help alleviate the client's anxiety.
b) Document that the client has expressed concerns about the surgery.
Documenting the client's concerns is important for accurate record-keeping and continuity of care. However, it should not be the only action taken. Notifying the charge nurse is crucial to ensure appropriate follow-up and support for the client.
d) Remind the client that the consent has already been obtained.
Reminding the client that they have already signed the informed consent may not effectively address their fears and concerns. Reassurance and support should be provided, and involving the charge nurse and healthcare team is essential to address the client's emotional well-being.
In summary, when a preoperative client confides in the practical nurse (PN) about being frightened and unsure about undergoing surgery, the priority action is to notify the charge nurse of the client's concerns. This allows for appropriate interventions, support, and coordination of care to address the client's fears, ensure their emotional well-being, and provide necessary information about the surgical procedure.
Correct Answer is A
Explanation
Choice A rationale:
The nurse should instruct the client to sleep with an extra pillow under their head. This position, known as the semi-Fowler's position, elevates the upper body and head, which can help reduce shortness of breath and difficulty breathing while lying down at night. Propranolol, a non-selective beta-blocker, can cause bronchoconstriction in some individuals, especially those with a history of respiratory issues. Elevating the head can assist in improving lung expansion and reducing the sensation of breathlessness.
Choice B rationale:
Sleeping on their left side would not be the best option in this case. While sleeping on the left side is often recommended for individuals with certain cardiac conditions to improve blood flow and reduce pressure on the heart, it may not be as effective for alleviating the respiratory symptoms caused by propranolol. Elevating the head is a more appropriate intervention in this scenario.
Choice C rationale:
Sleeping on their right side is not the ideal choice either. While it can have benefits for individuals with certain cardiac conditions, it does not address the specific respiratory symptoms reported by the client. Elevating the head is a more targeted intervention to alleviate breathlessness associated with propranolol.
Choice D rationale:
Sleeping on their back may worsen the client's symptoms. Lying flat on the back can lead to increased pressure on the diaphragm, making it more challenging to breathe for individuals experiencing shortness of breath. Therefore, it is not the recommended position for this client.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
