Which laboratory results should the nurse closely monitor in a client who has end-stage renal disease (ESRD)?
Blood pressure, heart rate, and temperature.
Leukocytes, neutrophils, and thyroxine.
Serum potassium, calcium, and phosphorus.
Erythrocytes, hemoglobin, and hematocrit.
The Correct Answer is C
Choice C reason: serum potassium, calcium, and phosphorus are electrolytes that can be affected by ESRD. ESRD is a condition in which the kidneys lose their ability to filter waste products and excess fluids from the blood. This can cause electrolyte imbalances that can lead to serious complications, such as cardiac arrhythmias, bone disorders, or metabolic acidosis. The nurse should closely monitor these electrolytes and report any abnormal values.
Choice A reason: blood pressure, heart rate, and temperature are vital signs that are not specific to ESRD. Vital signs can be influenced by many factors and may not reflect the severity of kidney damage. The nurse should monitor vital signs regularly, but not as closely as electrolytes.
Choice B reason: leukocytes, neutrophils, and thyroxine are not laboratory results that are directly related to ESRD. Leukocytes and neutrophils are types of white blood cells that are involved in immune response and inflammation. Thyroxine is a hormone that regulates metabolism and growth. These laboratory results may be altered by other conditions or medications, but not by ESRD.
Choice D reason: erythrocytes, hemoglobin, and hematocrit are laboratory results that measure the red blood cell count and oxygen-carrying capacity of the blood. These laboratory results may be decreased in ESRD due to anemia, which is a common complication of chronic kidney disease. However, anemia is not as life-threatening as electrolyte imbalances and can be treated with erythropoietin injections or iron supplements.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
Choice A reason: Marking an outline of the "olive-shaped" mass in the right epigastric area is not a priority nursing action. The mass is caused by hypertrophy of the pyloric sphincter, which obstructs gastric emptying and causes projectile vomiting. The mass may not be palpable in all cases.
Choice B reason: This is the correct answer because maintaining a continuous infusion of IV fluids per prescription is essential to prevent dehydration and electrolyte imbalance in the infant. The infant may have significant fluid loss due to vomiting and poor intake.
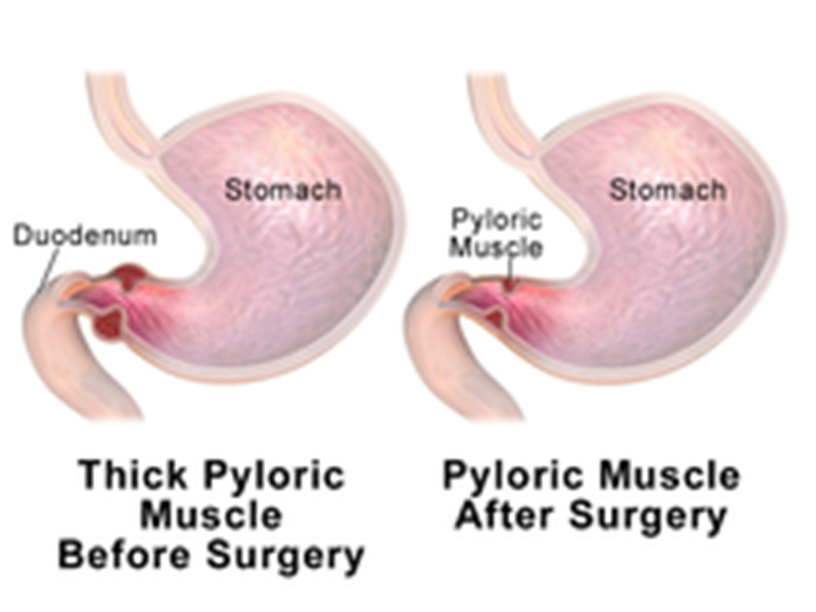
Choice C reason: Monitoring amount of intake and infant's response to feedings is important, but not the highest priority. The infant may have difficulty feeding due to nausea, vomiting, and abdominal pain.
Choice D reason: Instructing parents regarding care of the incisional area is a post-operative nursing action, not a pre-operative one. The parents will need to learn how to keep the incision clean and dry, monitor for signs of infection, and administer pain medication as prescribed.
Correct Answer is C
Explanation
Choice A reason: When the client has ankle edema is not the most important time for the nurse to assess DTRs, as this is a common finding in pregnancy and does not indicate a neurological or vascular problem. This is a distractor choice.
Choice B reason: Within the first trimester of pregnancy is not the most important time for the nurse to assess DTRs, as this is a routine assessment that can be done at any time during pregnancy and does not reflect any specific risk or complication. This is another distractor choice.
Choice C reason: If the client has an elevated blood pressure is the most important time for the nurse to assess DTRs, as this can indicate preeclampsia, a serious condition that can cause seizures, stroke, and organ damage. DTRs can help detect hyperreflexia, which is a sign of increased intracranial pressure and impending eclampsia. Therefore, this is the correct choice.
Choice D reason: During admission to labor and delivery is not the most important time for the nurse to assess DTRs, as this is a standard assessment that can be done at any stage of labor and does not signify any urgent or emergent situation. This is another distractor choice.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
