Which of the following tube additives promotes clot formation?
Heparin
Oxalate
Citrate
Silica
The Correct Answer is D
Choice A reason:
Heparin is an anticoagulant, not a clot activator. It works by inhibiting thrombin and preventing the conversion of fibrinogen to fibrin, thus preventing clot formation. It is commonly found in green-top tubes and is suitable for collecting plasma samples for tests like electrolyte levels and coagulation studies.
Choice B reason:
Oxalate is also an anticoagulant that prevents clotting by precipitating calcium. It is not used to promote clot formation but rather to maintain a blood sample in a non-coagulated state for various tests.
Choice C reason:
Citrate functions similarly to heparin and oxalate as an anticoagulant. It chelates calcium ions in the blood, inhibiting the coagulation process. Citrate is often used in blue-top tubes and is ideal for collecting plasma samples for coagulation studies.
Choice D reason:
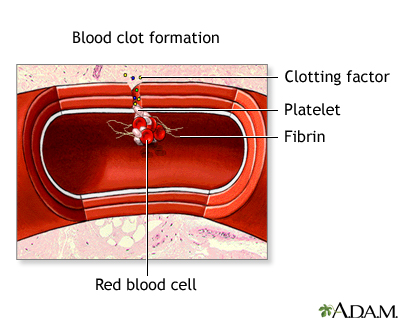
Silica is a clot activator. It is commonly used in serum separator tubes (SSTs) with a gold or red speckled top. The silica particles provide a surface for the rapid formation of the clot, allowing for the separation of serum from the blood cells. This is essential when serum is needed for testing.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
Choice A Reason:
Using only one patient identifier is not sufficient to ensure patient safety and accuracy in healthcare settings. It increases the risk of misidentification, which can lead to serious medical errors. Therefore, one identifier is not the standard practice for patient verification before a blood draw.
Choice B Reason:
While two identifiers are commonly used in many healthcare settings as a minimum requirement, they may not always provide enough differentiation, especially in larger facilities where patient names may be similar. Two identifiers are often the minimum standard, but they are not the most comprehensive approach.
Choice C Reason:
Three unique patient identifiers provide a more robust method for verifying a patient's identity, significantly reducing the likelihood of errors. According to the Clinical and Laboratory Standards Institute (CLSI), three identifiers are recommended to ensure the correct patient is being collected. This may include the patient's full name, date of birth, and medical record number or another unique identifier.
Choice D Reason:
While using four unique identifiers could further reduce the risk of patient misidentification, it is not typically required as the standard minimum. Three identifiers are generally considered adequate for most healthcare settings to ensure patient safety and proper identification.
Correct Answer is B
Explanation
Choice A reason:
Using a needle at a 45° angle does not typically result in collapsing the vein. A collapsed vein is more likely due to excessive vacuum pressure from the tube, a very small or fragile vein, or the tourniquet being too tight.
Choice B reason:
At a 45° angle, the needle is more likely to penetrate through the entire depth of the vein, especially if the vein is superficial. This can result in a failed venipuncture because the needle has entered and exited the vein, missing the opportunity to collect blood.
Choice C reason:
While a steep angle like 45° could cause the needle to miss the vein superficially, it is more likely that the needle would go through the vein at this angle rather than merely missing it superficially. A superficial miss is more likely with an angle that is too shallow.
Choice D reason:
Contacting the upper wall of the vein alone would not necessarily result in a failed venipuncture. However, at a 45° angle, the needle could easily slip through the vein entirely after contacting the upper wall, especially if the vein is not anchored well.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
