A client in the recovery room following a procedure is unable to void, so the nurse obtains a prescription to perform a straight catheterization. After inserting the catheter, the nurse observes that the client has an immediate output of 500 mL of clear yellow urine. Which action should the nurse implement next?
Remove the catheter and palpate the client's bladder for residual distention.
Remove the catheter and replace with an indwelling catheter.
Allow the bladder to empty completely or up to 1,000 mL of urine.
Clamp the catheter for thirty minutes and then resume draining.
The Correct Answer is C
Choice A: Remove the catheter and palpate the client's bladder for residual distention. This is not the best action, as it may cause discomfort and trauma to the client. The catheter should not be removed until the bladder is fully emptied or up to 1,000 mL of urine is drained, as removing it too soon may cause urinary retention or infection.
Choice B: Remove the catheter and replace with an indwelling catheter. This is not the best action, as it may cause unnecessary exposure and trauma to the client. The catheter should not be replaced unless ordered by the healthcare provider, as replacing it may increase the risk of infection or urethral injury.
Choice C: Allow the bladder to empty completely or up to 1,000 mL of urine. This is the best action, as it can prevent bladder spasms, overdistention, or rupture. The nurse should monitor the urine output and color, and document the amount and characteristics of urine drained.
Choice D: Clamp the catheter for thirty minutes and then resume draining. This is not the best action, as it may cause pain and discomfort to the client. The catheter should not be clamped unless ordered by the healthcare provider, as clamping it may increase the risk of infection or bladder damage.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
Choice A: Increasing oxygen to 6 liters/minute is not an intervention that the nurse should implement, as this can worsen bronchospasm and hypoxia by reducing the hypoxic drive and causing carbon dioxide retention. This is a contraindicated choice.
Choice B: Calling for an Ambu resuscitation bag is not an intervention that the nurse should implement, as this is not indicated for a client who is conscious and breathing spontaneously. This is an overreaction choice.
Choice C: Instructing the client to lie back in bed is not an intervention that the nurse should implement, as this can increase respiratory distress and compromise airway clearance by reducing lung expansion and increasing abdominal pressure. This is another contraindicated choice.
Choice D: Administering a nebulizer treatment is an intervention that the nurse should implement, as this can deliver bronchodilators and anti-inflammatory agents directly to the airways and improve ventilation and oxygenation for this client. Therefore, this is the correct choice.
Correct Answer is D
Explanation
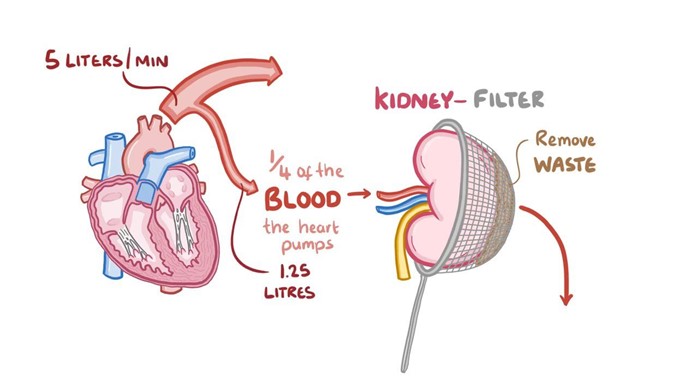
Choice A: Assessing pupillary response to light hourly is not an intervention that the nurse should implement while administering dopamine, as this is not related to the effects or side effects of dopamine. This is a distractor choice.
Choice B: Initiating seizure precautions is not an intervention that the nurse should implement while administering dopamine, as this is not a common or expected complication of dopamine. This is another distractor choice.
Choice C: Monitoring serum potassium frequently is not an intervention that the nurse should implement while administering dopamine, as this is not affected by dopamine or hypotension. This is another distractor choice.
Choice D: Measuring urinary output every hour is an intervention that the nurse should implement while administering dopamine, as this can indicate the effectiveness of dopamine in improving renal perfusion and blood pressure. Therefore, this is the correct choice.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
