A client who had a biliopancreatic diversion procedure (BPD) 3 months ago is admitted with severe dehydration. Which assessment finding warrants immediate intervention by the nurse?
Gastroccult positive emesis.
Strong foul smelling flatus.
Complaint of poor night vision.
Loose bowel movements.
The Correct Answer is A
Choice A reason: Gastroccult positive emesis indicates the presence of blood in the vomit, which is a sign of a serious complication such as anastomotic leak, ulcer, or bleeding. The nurse should notify the physician and monitor the client's vital signs and hemoglobin level.
Choice B reason: Strong foul smelling flatus is a common side effect of BPD, which involves bypassing a large portion of the small intestine and creating a connection between the stomach and the colon. This results in malabsorption and bacterial overgrowth, which produce gas and odor.
Choice C reason: Complaint of poor night vision is a sign of vitamin A deficiency, which can occur after BPD due to reduced absorption of fat-soluble vitamins. The nurse should advise the client to take vitamin supplements and eat foods rich in vitamin A, such as carrots, sweet potatoes, and spinach.
Choice D reason: Loose bowel movements are another common side effect of BPD, which causes diarrhea and steatorrhea (fatty stools). The nurse should encourage the client to drink fluids with electrolytes and avoid foods that worsen diarrhea, such as greasy, spicy, or sugary foods.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
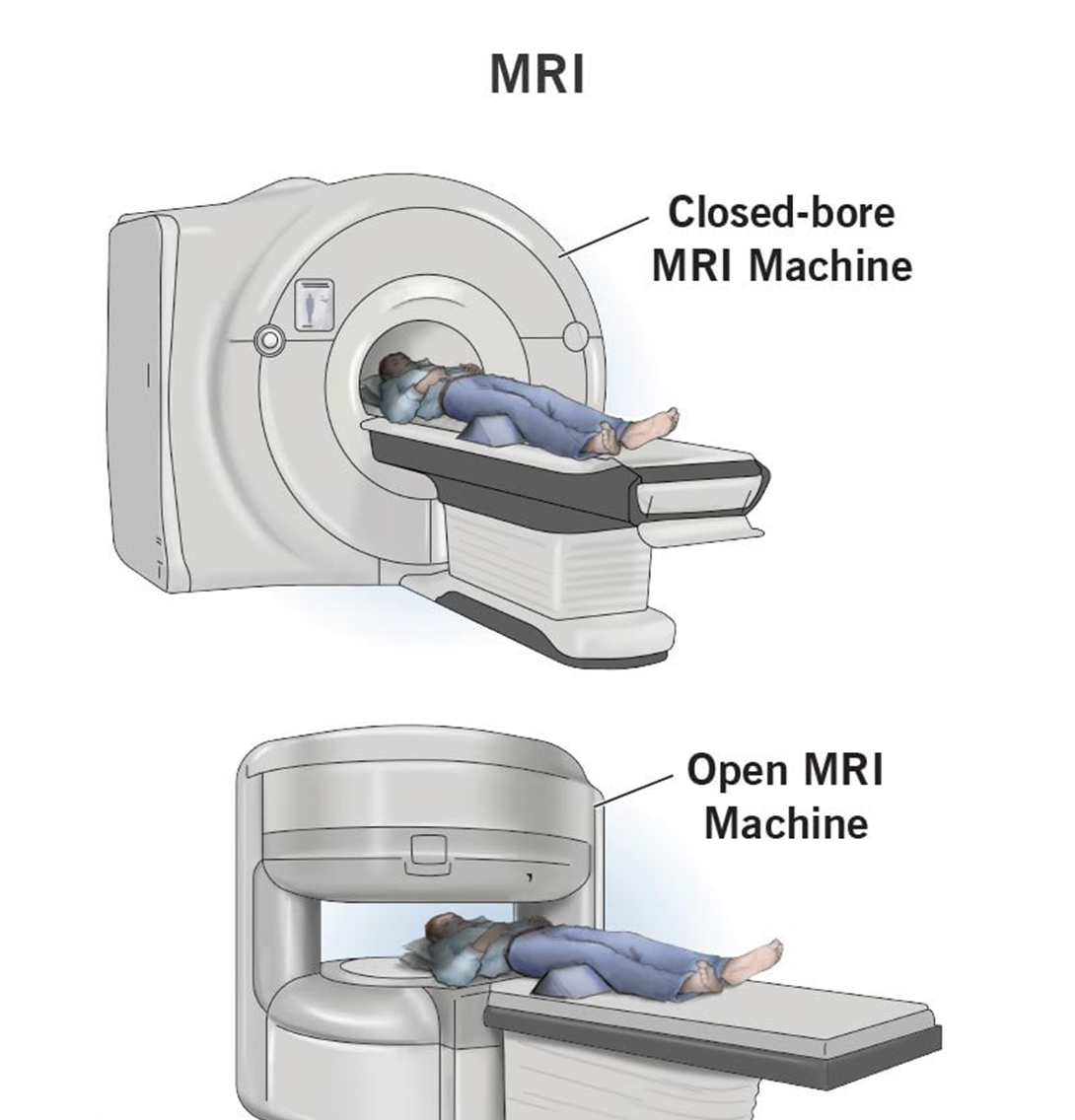
Choice A reason: Fasting blood sugar of 200 mg/dL (11.1 mmol/L) indicates hyperglycemia, which is a high level of glucose in the blood. It can be caused by diabetes mellitus, stress, infection, or medication. Hyperglycemia can cause symptoms such as thirst, hunger, frequent urination, fatigue, and blurred vision. However, it does not affect the safety or accuracy of MRI with contrast.
Choice B reason: Glycosylated hemoglobin A1c of 8% indicates poor glycemic control over the past three months. It can be caused by diabetes mellitus, chronic kidney disease, or hemoglobinopathy. Glycosylated hemoglobin A1c reflects the average blood glucose level over the lifespan of red blood cells, which is about 120 days. However, it does not affect the safety or accuracy of MRI with contrast.
Choice C reason: Blood urea nitrogen of 22 mg/dL (7.9 mmol/L) indicates mild azotemia, which is a high level of nitrogenous waste products in the blood. It can be caused by dehydration, high protein intake, gastrointestinal bleeding, or kidney impairment. Azotemia can cause symptoms such as nausea, vomiting, confusion, and lethargy. However, it does not affect the safety or accuracy of MRI with contrast.
Choice D reason: Serum creatinine of 1.9 mg/dL (169 umol/L) indicates moderate renal insufficiency, which is a reduced ability of the kidneys to filter and excrete waste products and fluids from the body. It can be caused by diabetes mellitus, hypertension, glomerulonephritis, or nephrotoxic drugs. Renal insufficiency can cause symptoms such as edema, anemia, electrolyte imbalance, and acidosis. It can also increase the risk of contrast-induced nephropathy, which is a sudden deterioration of kidney function after exposure to contrast media used for imaging studies such as MRI. Contrast-induced nephropathy can lead to acute kidney injury, dialysis requirement, or even death. Therefore, serum creatinine should be reported to the healthcare provider before MRI with contrast to assess the risk and benefit of the procedure and to take preventive measures such as hydration, medication adjustment, or alternative imaging modalities.
Correct Answer is A
Explanation
Choice A reason: This is correct because performing a bedside pregnancy test is the intervention that should be implemented immediately by the nurse. This is to confirm or rule out pregnancy and inform the surgical team of any possible risks or complications that may affect the client or the fetus.
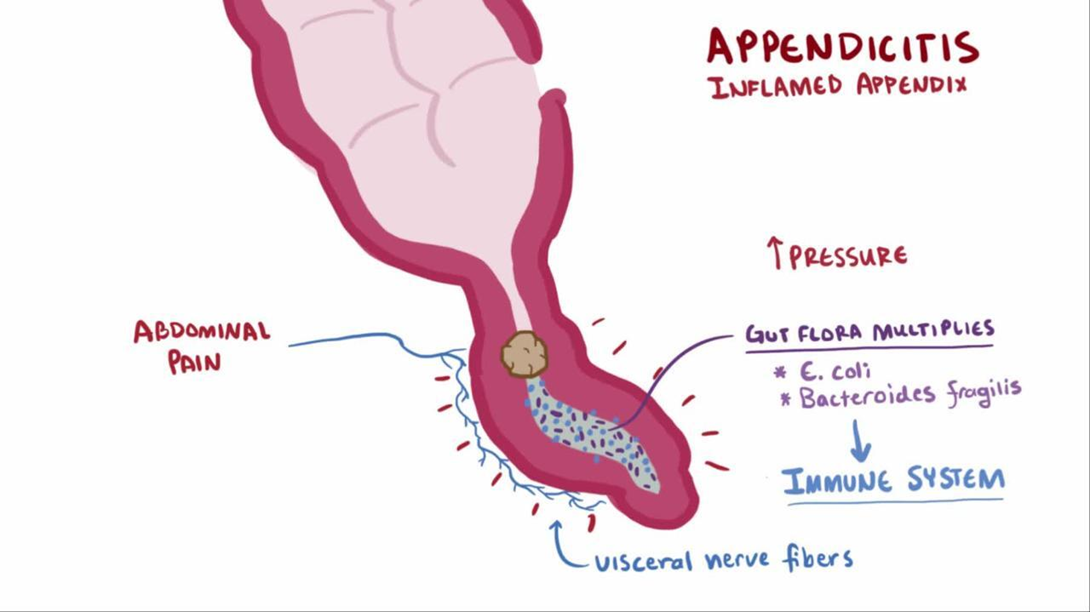
Choice B reason: This is incorrect because continuing with surgery as scheduled is not an appropriate intervention without verifying the pregnancy status of the client. Surgery may pose serious threats to both maternal and fetal health, such as bleeding, infection, anesthesia complications, or miscarriage.
Choice C reason: This is incorrect because calculating gestation from last menstrual cycle is not an accurate or reliable method of determining pregnancy. The menstrual cycle can vary widely among women and may be affected by various factors such as stress, illness, or medication.
Choice D reason: This is incorrect because notifying the surgical team to cancel the surgery is not a necessary intervention unless pregnancy is confirmed. Appendicitis is a medical emergency that requires prompt surgical treatment to prevent rupture, peritonitis, or sepsis.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
